Ozempic Constipation: Relief Strategies That Actually Work

If you’re dealing with constipation on Ozempic, you’re probably tired of generic advice like “drink more water” without real solutions that address the specific challenges this medication creates. Maybe you’ve gone days without a bowel movement, feel uncomfortably bloated, or you’re frustrated that the very medication helping you lose weight is causing this particular misery.
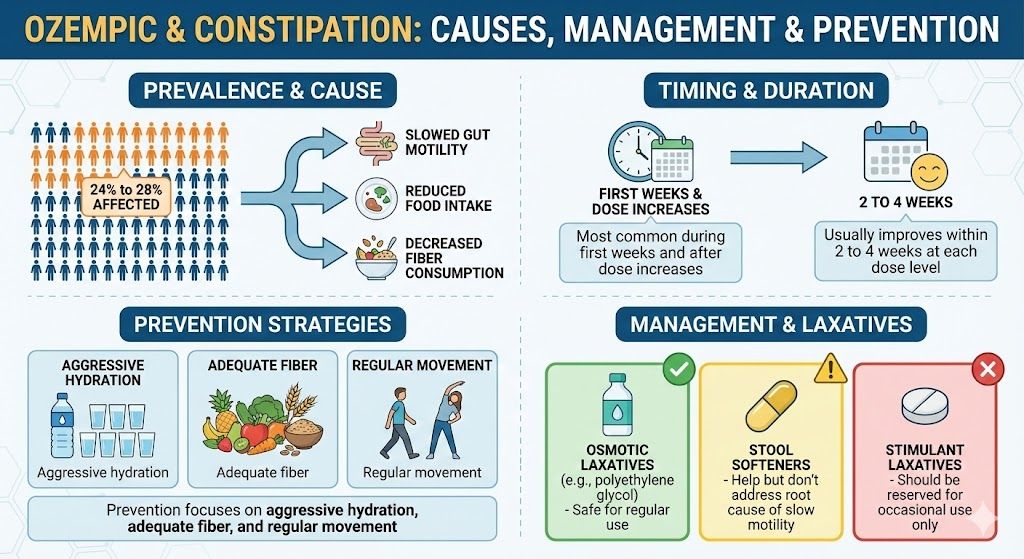
Here’s what you need to know: constipation affects approximately 24% to 28% of people taking Ozempic, making it one of the more common side effects. It’s caused by a combination of dramatically slowed gut motility from the medication, eating significantly less food overall (meaning less material moving through your digestive system), consuming less fiber as appetite disappears, and often being mildly dehydrated. While uncomfortable and sometimes painful, Ozempic constipation is manageable with the right combination of prevention strategies and effective treatments.
This guide provides specific, actionable solutions for preventing and relieving constipation on Ozempic. You’ll learn exactly why this happens, proven strategies that work better than generic advice, when constipation requires medical attention, and how to manage this side effect long-term.
Key Takeaways: Ozempic and Constipation
- Constipation affects 24% to 28% of people taking Ozempic
- Caused by slowed gut motility, reduced food intake, and decreased fiber consumption
- Most common during first weeks and after dose increases
- Usually improves within 2 to 4 weeks at each dose level
- Prevention focuses on aggressive hydration, adequate fiber, and regular movement
- Osmotic laxatives like polyethylene glycol are safe for regular use
- Stool softeners help but don’t address root cause of slow motility
- Stimulant laxatives should be reserved for occasional use only
Why Ozempic Causes Constipation
Understanding the specific mechanisms behind Ozempic-related constipation helps you address it more effectively than generic constipation remedies.
Slowed Gut Motility Throughout Digestive Tract
Ozempic’s primary mechanism is activating GLP-1 receptors throughout your digestive system. While the slowed gastric emptying gets the most attention (because it contributes to feeling full), GLP-1 receptors exist throughout your entire intestinal tract. Activating these receptors slows the movement of contents through your small intestine and colon, not just your stomach.
Think of your digestive system like a conveyor belt. Normally, coordinated muscle contractions (called peristalsis) move food and waste through at a steady pace. Ozempic slows this conveyor belt significantly. Food moves through more slowly, and waste sits in your colon longer.
When waste material sits in your colon for extended periods, more water gets absorbed from it. This makes stools harder and drier, which makes them more difficult to pass. The longer the transit time, the worse this effect becomes.
Dramatically Reduced Food Intake
Ozempic’s powerful appetite suppression often causes people to eat 50% to 70% less food than before treatment. While this caloric reduction drives weight loss, it also means you’re physically putting less material into your digestive system.
Less food going in inevitably means less waste coming out. If you’re eating 1,200 calories daily instead of 2,500, you’re consuming roughly half the volume of food. This naturally leads to less frequent bowel movements.
This isn’t necessarily problematic constipation if you’re still having comfortable bowel movements, just less frequently. However, when combined with slowed motility, reduced food intake can tip into actual constipation with hard stools and discomfort.
Decreased Fiber Consumption
When appetite disappears and eating becomes a chore, many people gravitate toward simple, easy-to-consume foods. Crackers, toast, plain pasta, and rice go down easier when you’re not hungry compared to high-fiber vegetables, beans, or whole grains.
Additionally, when you’re eating less total food, you’re naturally consuming less fiber even if your diet composition stays the same. If you previously ate 25 grams of fiber daily and now eat half as much food, you might only get 12 to 13 grams of fiber.
Fiber adds bulk to stool and helps it move through your intestines. Insufficient fiber, especially when gut motility is already slowed, significantly worsens constipation.
Dehydration
Many people don’t drink enough water while taking Ozempic. When you’re eating less, you’re also getting less fluid from food. When nausea is an issue, drinking might make you feel uncomfortably full.
Dehydration worsens constipation because your colon absorbs more water from stool to compensate for your body’s fluid needs. The result is harder, drier stools that are difficult to pass.
Even mild dehydration that doesn’t cause obvious symptoms elsewhere can significantly impact bowel function.
Reduced Physical Activity
Some people experience fatigue on Ozempic, particularly during initial adjustment periods. This might lead to less physical activity. Movement stimulates gut motility through mechanical effects and hormonal signaling. When you’re less active, your gut becomes less active too.
Additionally, rapid weight loss sometimes causes people to reduce exercise temporarily while their body adjusts. This activity reduction can contribute to constipation.
For comprehensive information about all Ozempic side effects, see our complete guide to semaglutide side effects.
When Constipation Typically Occurs
Understanding the timeline helps you anticipate and address constipation proactively.
First Few Weeks of Treatment
Constipation commonly develops within the first 1 to 3 weeks after starting Ozempic. Your digestive system is encountering dramatically slowed motility for the first time. You’re suddenly eating much less food. Your body hasn’t yet adapted to these changes.
You might notice that bowel movements become less frequent, going from daily to every 2 to 3 days. Stools become harder and require more straining. Bloating and abdominal discomfort develop. You feel like you need to go but can’t fully evacuate.
Not everyone experiences constipation during these first weeks. Some people maintain normal bowel function while others develop problems quickly.
After Dose Increases
Each time you increase your Ozempic dose, constipation might return or worsen even if it had improved at your previous dose. Higher doses create even slower gut motility. Appetite suppression strengthens, often leading to eating even less food.
The pattern mirrors other side effects: worst during the first 1 to 2 weeks at the new dose, gradual improvement over weeks 2 to 3, often resolution or significant improvement by week 4 at the same dose level.
Ongoing Pattern at Stable Doses
After adapting to a stable dose for several weeks, many people find that bowel function partially normalizes, though it typically doesn’t return completely to pre-treatment patterns. You might settle into a new normal of bowel movements every 2 to 3 days instead of daily, but they’re comfortable and don’t require straining.
Some people continue struggling with constipation throughout treatment despite implementing all recommended strategies. This persistent pattern can be frustrating and might influence long-term treatment decisions.
Interestingly, Some People Alternate
A subset of people experience alternating constipation and diarrhea. They might be constipated for several days, then have loose stools, then become constipated again. This pattern can be particularly frustrating to manage.
The alternating pattern often relates to the use of laxatives to address constipation, which then over-correct and cause loose stools, followed by a rebound into constipation.
Prevention Strategies: Stopping Constipation Before It Starts
Preventing constipation works much better than trying to fix it after you’re already miserable.
Aggressive Hydration
This is the single most important prevention strategy. Don’t just drink “more water.” Be systematic and aggressive about hydration. Aim for at least 80 to 100 ounces of water daily, significantly more than the standard 64-ounce recommendation.
Carry a large water bottle everywhere and sip constantly throughout the day. Set phone reminders every hour to drink. Track your intake using an app if that helps you stay accountable.
Don’t wait until you feel thirsty. By the time thirst registers, you’re already mildly dehydrated. Make hydration a conscious priority from day one of Ozempic treatment.
Warm or room temperature water often sits better than very cold water when you’re experiencing other GI side effects. Consider adding electrolyte packets occasionally to support hydration, especially if you exercise.
Prioritize Fiber from Day One
Don’t wait for constipation to develop before addressing fiber intake. Proactively increase fiber as you start Ozempic. Aim for 25 to 35 grams of fiber daily even though you’re eating less food overall. This means choosing fiber-rich foods as a higher percentage of your reduced caloric intake.
Include vegetables at most meals, even if portions are small. Berries, apples, and pears provide fiber in easily consumable portions. Choose whole grains over refined grains when you eat bread, rice, or pasta. Add beans or lentils to meals when possible. Consider a fiber supplement like psyllium husk (Metamucil) or methylcellulose (Citrucel) if you struggle to get adequate fiber from food.
When adding fiber, increase gradually over days to weeks rather than jumping from 10 grams to 35 grams overnight. Rapid fiber increases can cause gas, bloating, and paradoxically worsen constipation if you’re not drinking enough water. Fiber needs adequate water to work properly.
Stay Physically Active
Regular movement stimulates gut motility. Even gentle activity helps. Walk for 20 to 30 minutes daily, ideally after meals when movement has the most beneficial effect on digestion. Include some form of physical activity most days, whether that’s structured exercise or just staying generally active throughout the day.
You don’t need intense workouts. Moderate walking, yoga, swimming, or cycling all support digestive function. The key is consistency rather than intensity.
Don’t Restrict Food Too Severely
Despite reduced appetite, ensure you’re eating at least 1,200 to 1,500 calories daily. Very low calorie intake means too little material moving through your digestive system. Your gut needs a certain volume of food to stimulate peristalsis.
Focus on nutrient-dense, fiber-rich foods even when you’re not hungry. Make every calorie count by choosing foods that support digestive health rather than empty calories.
Establish a Bathroom Routine
Your colon responds to routine. Try to have a consistent time for attempting a bowel movement, ideally in the morning about 20 to 30 minutes after breakfast or coffee. The gastrocolic reflex (your colon’s response to eating) is strongest in the morning.
Don’t ignore the urge when it comes. Delaying bowel movements when you feel the need can worsen constipation over time.
Consider a Daily Stool Softener
Taking a stool softener like docusate sodium (Colace) daily from the beginning of treatment can help prevent constipation from developing. These are gentle, safe for long-term use, and help keep stools soft as they move through your slowed digestive system.
Typical dose is 100 to 200 mg daily. They work by allowing more water to mix with stool, keeping it soft. They don’t stimulate bowel movements, so they won’t cause urgency or cramping.
Add Healthy Fats
While you might be reducing overall fat intake for weight loss, don’t eliminate fats entirely. Healthy fats help lubricate your digestive system and support bowel function. Include olive oil in cooking or on salads. Eat avocados regularly if you tolerate them. Include nuts or nut butters in small amounts. Add ground flaxseed to foods (which provides both healthy fat and fiber).
Fats also slow gastric emptying, but in the context of constipation, the lubricating effect is beneficial.
Effective Relief Strategies When Constipation Occurs
Despite prevention efforts, constipation might still develop. These treatments provide relief ranked from gentlest to strongest.
First Line: Osmotic Laxatives
Polyethylene glycol (MiraLAX, GlycoLax) is the gold standard for treating constipation on Ozempic. This osmotic laxative works by drawing water into your colon, softening stool and stimulating bowel movements. It’s safe for daily use, doesn’t cause dependency, doesn’t cause cramping or urgency in most people, and is gentle and effective.
Take one dose (usually 17 grams powder dissolved in 8 oz of liquid) daily, preferably at the same time each day. It typically produces a bowel movement within 1 to 3 days. If constipation is severe, you can take it twice daily initially.
Other osmotic laxatives include magnesium citrate (stronger effect but can cause cramping), lactulose (prescription, very effective but can cause gas), and sorbitol (works similarly to lactulose).
Polyethylene glycol is available over-the-counter, inexpensive, and should be your go-to treatment for Ozempic-related constipation.
Stool Softeners
If you’re not already taking a daily stool softener, start one immediately when constipation develops. Docusate sodium (Colace) at 100 to 200 mg twice daily helps soften existing hard stool. These work best for prevention and mild constipation rather than severe impaction.
Combine stool softeners with osmotic laxatives for best results. The stool softener makes stool easier to pass while the osmotic laxative helps move it through.
Magnesium Supplements
Magnesium in any form tends to have a laxative effect. Magnesium citrate is specifically marketed as a laxative and works quickly, usually within 6 hours. Magnesium oxide has a strong laxative effect. Magnesium glycinate is gentler if you just want mild support. Typical dose for laxative effect is 400 to 800 mg daily.
Be aware that excessive magnesium can cause diarrhea. Start with lower doses and increase as needed. Don’t take magnesium if you have kidney problems without consulting your provider.
Increase Fiber Temporarily
If you haven’t been prioritizing fiber, dramatically increase it when constipation strikes. Add a fiber supplement immediately, take it 2 to 3 times daily with plenty of water, increase vegetable and fruit consumption, add prunes or prune juice which have natural laxative properties, and try ground flaxseed added to foods.
Remember that fiber requires adequate water to work properly. Increasing fiber without sufficient hydration can actually worsen constipation.
Stimulant Laxatives (Use Sparingly)
Stimulant laxatives like bisacodyl (Dulcolax) or senna (Senokot) should be reserved for severe constipation or when other approaches haven’t worked. These medications stimulate intestinal contractions, forcing bowel movements. They work quickly, usually within 6 to 12 hours. However, they can cause cramping and urgency, can lead to dependency if used regularly, and aren’t appropriate for long-term daily use.
Use stimulant laxatives occasionally when you’re truly constipated and other gentler approaches haven’t worked within 3 to 4 days. Don’t rely on them regularly.
Enemas or Suppositories
For severe constipation or impaction, enemas or glycerin suppositories provide quick relief. These work locally in the rectum and lower colon to stimulate evacuation. They’re safe for occasional use when oral treatments haven’t worked or when you need fast relief.
Follow package directions carefully. These are emergency measures rather than regular solutions.
Adequate Water with All Treatments
Whatever constipation treatment you use, drink plenty of water throughout the day. Laxatives work by drawing or pushing water into your colon. If you’re dehydrated, they can’t work effectively and might even worsen discomfort.
Aim for 80 to 100 ounces of water daily when actively treating constipation.
For information about managing nausea alongside constipation, see our guide to Ozempic nausea management.
What Works Best: A Practical Protocol
Based on clinical experience and patient reports, here’s the most effective approach to managing Ozempic constipation.
For Prevention (Start from Day One)
Drink 80 to 100 ounces of water daily, distributed throughout the day. Take 100 to 200 mg of docusate sodium (Colace) daily. Consume 25 to 35 grams of fiber daily through food and supplements. Walk for 20 to 30 minutes daily. Include healthy fats in your diet regularly.
For Mild Constipation (No Bowel Movement for 2 to 3 Days)
Continue all prevention strategies. Add polyethylene glycol (MiraLAX) once daily. Increase water intake to 100+ ounces daily. Add prunes or prune juice. Take a 20 to 30 minute walk after each meal if possible.
For Moderate Constipation (No Bowel Movement for 3 to 5 Days, Discomfort)
Continue all above strategies. Increase polyethylene glycol to twice daily. Add magnesium citrate 400 to 800 mg daily. Consider a gentle stimulant laxative if no movement by day 5. Stay very well hydrated with 100+ ounces of water.
For Severe Constipation (More Than 5 Days, Severe Discomfort, Bloating)
All above strategies plus consider a stimulant laxative if needed. Use an enema or suppository if oral treatments haven’t worked. Contact your healthcare provider if no relief within 24 hours of aggressive treatment. Watch for warning signs requiring immediate attention (see below).
Long-Term Maintenance Once Regular Again
Continue drinking 80 to 100 ounces of water daily. Take daily stool softener indefinitely while on Ozempic. Maintain high fiber intake (25 to 35 grams daily). Use polyethylene glycol 3 to 4 times weekly or daily as needed to maintain regularity. Stay physically active. Don’t let yourself go more than 2 to 3 days without a bowel movement before intervening.
When Constipation Requires Medical Attention
Most constipation is uncomfortable but not dangerous. However, certain situations warrant immediate medical evaluation.
Seek Immediate Medical Attention If You Experience
Severe abdominal pain, particularly if sharp, constant, or worsening. Abdominal distension (swelling) that’s severe or rapidly worsening. Vomiting, especially if you also haven’t had a bowel movement in several days. Blood in your stool (unless you have known hemorrhoids and it’s a small amount). Complete inability to pass gas or stool (possible bowel obstruction). Fever above 100.4°F with constipation. Severe nausea with constipation and abdominal pain.
These symptoms might indicate bowel obstruction, severe impaction, or other conditions requiring urgent evaluation and treatment.
Contact Your Provider (Less Urgent but Important) If
Constipation persists despite aggressive treatment with multiple interventions for more than 7 to 10 days. You develop severe hemorrhoids or rectal bleeding from straining. Constipation significantly worsens at each dose increase rather than improving with adaptation. You need stimulant laxatives regularly to have bowel movements. Over-the-counter treatments aren’t providing adequate relief.
Your provider might suggest prescription medications, dose adjustments to Ozempic, evaluation for underlying issues, or additional interventions.
Foods That Help vs Foods That Worsen Constipation
Strategic food choices significantly impact bowel function on Ozempic.
Foods That Help Constipation
Prunes and prune juice contain sorbitol, a natural laxative, plus fiber. Berries (raspberries, blackberries, strawberries) provide significant fiber in small volumes. Leafy greens like spinach, kale, and Swiss chard offer fiber and magnesium. Beans and lentils pack impressive fiber and protein. Flaxseeds (ground) provide both fiber and healthy fats that support bowel movements.
Chia seeds absorb water and add bulk to stool. Pears and apples with skin contain soluble and insoluble fiber. Sweet potatoes provide fiber and are easily digestible. Avocados offer healthy fats and fiber. Whole grains like oatmeal, brown rice, and whole wheat bread provide sustained fiber. Kefir and yogurt contain probiotics supporting gut health.
Foods That Worsen Constipation
White bread, white rice, and refined pasta lack fiber and can slow digestion. Processed foods often lack fiber and contain additives that can worsen constipation. Excessive dairy (cheese particularly) can be constipating for many people. Red meat can be difficult to digest and slows gut transit. Fried and fatty foods slow digestion even further beyond Ozempic’s effects. Bananas (especially unripe) can be constipating due to resistant starch. Chocolate contains compounds that can slow gut motility.
You don’t need to completely avoid these foods, but minimize them when you’re struggling with constipation.
Comparing Constipation Across GLP-1 Medications
Understanding how Ozempic’s constipation risk compares to similar medications provides useful context.
Ozempic vs Mounjaro/Zepbound (Tirzepatide)
Tirzepatide causes constipation at similar rates to semaglutide, affecting 20% to 25% of users. The dual GLP-1/GIP mechanism creates similar gut motility slowing. Some people report that tirzepatide causes more overall digestive side effects including constipation, though individual responses vary tremendously.
Interestingly, tirzepatide users report diarrhea slightly more frequently than semaglutide users, but constipation rates are comparable. Some people who struggled with constipation on semaglutide do better on tirzepatide and vice versa, but there’s no clear pattern predicting who will do better on which medication.
For detailed comparison, see our Mounjaro vs Ozempic guide.
Ozempic vs Saxenda (Liraglutide)
Liraglutide requires daily injections rather than weekly. Constipation rates are similar to semaglutide, around 20% to 25%. The daily dosing versus weekly doesn’t meaningfully affect constipation patterns since both medications work continuously once they reach steady state levels.
Ozempic vs Wegovy
These contain the same active ingredient (semaglutide), just at different doses and approved for different indications (diabetes vs weight loss). Constipation risk is identical between them.
Long-Term Considerations and Adaptations
After months on Ozempic, constipation patterns often evolve.
Many People Adapt
After 6 to 12 months at a stable maintenance dose, many people find that bowel function partially normalizes. You might settle into a pattern of comfortable bowel movements every 2 to 3 days instead of daily, which is perfectly healthy if stools remain soft and easy to pass.
Your gut bacteria adapt to the medication’s effects. Your body adjusts to operating on less food volume. You’ve likely optimized your prevention strategies. The result is often less problematic constipation even though gut motility remains slower than pre-treatment.
Some Require Ongoing Management
A subset of people need continued daily interventions to maintain comfortable bowel function throughout Ozempic treatment. Daily stool softeners, regular polyethylene glycol use several times weekly, strict adherence to high fiber and hydration, and regular physical activity become permanent lifestyle elements.
This ongoing management is usually manageable but requires commitment. For most people, the weight loss and health benefits justify the constipation management effort.
Consider Periodic Reassessment
If constipation remains severe and quality-of-life-impairing despite all interventions, periodic reassessment with your provider makes sense. Options might include trying a different GLP-1 medication to see if you respond better, staying at a lower dose where side effects are more manageable, taking periodic breaks from treatment (though this causes weight regain), or considering alternative weight loss approaches.
For information about what happens after stopping Ozempic, see our guide to how long semaglutide stays in your system.
Frequently Asked Questions
How common is constipation on Ozempic?
Constipation affects approximately 24% to 28% of people taking Ozempic based on clinical trial data. This makes it one of the more common side effects, occurring at similar rates to nausea and diarrhea. However, most people don’t experience it, and those who do often find it improves significantly within 2 to 4 weeks at each dose level as their body adapts.
Why does Ozempic cause constipation?
Ozempic activates GLP-1 receptors throughout your digestive tract, significantly slowing gut motility and the movement of contents through your intestines. This allows more water to be absorbed from stool, making it harder and more difficult to pass. Additionally, dramatically reduced food intake means less material moving through your system, and decreased fiber consumption worsens the problem. The combination of slower motility, less food volume, and less fiber creates ideal conditions for constipation.
What is the best laxative to use with Ozempic?
Polyethylene glycol (MiraLAX) is the most effective and safest laxative for managing Ozempic-related constipation. It’s an osmotic laxative that draws water into your colon, softening stool and stimulating bowel movements. It’s safe for daily long-term use, doesn’t cause dependency or cramping, and works gently over 1 to 3 days. Take 17 grams dissolved in 8 oz of liquid once or twice daily as needed to maintain comfortable bowel function.
Does constipation from Ozempic go away?
For most people, constipation improves significantly within 2 to 4 weeks at each dose level as the digestive system adapts. It’s typically worst during the first weeks of treatment and after dose increases, then gradually improves. After several months at a stable maintenance dose, many people experience normal or near-normal bowel function, though it may not return completely to pre-treatment patterns. Some people continue requiring ongoing management strategies throughout treatment.
How can I prevent constipation on Ozempic?
Effective prevention strategies include drinking 80 to 100 ounces of water daily distributed throughout the day, consuming 25 to 35 grams of fiber daily through food and supplements, taking a daily stool softener (docusate sodium 100 to 200 mg) starting from day one, staying physically active with at least 20 to 30 minutes of walking daily, ensuring adequate food intake (at least 1,200 to 1,500 calories), and including healthy fats in your diet regularly. Prevention works much better than treating constipation after it develops.
Can I take MiraLAX every day on Ozempic?
Yes, polyethylene glycol (MiraLAX) is safe for daily long-term use. Unlike stimulant laxatives that can cause dependency, osmotic laxatives like polyethylene glycol simply draw water into your colon to soften stool. Many people on Ozempic use it daily or several times weekly throughout treatment to maintain comfortable bowel function. It’s gentle, effective, and doesn’t lose effectiveness over time.
What foods help with Ozempic constipation?
Foods that significantly help include prunes and prune juice (natural laxative effect), berries which provide fiber in small portions, leafy greens offering fiber and magnesium, beans and lentils packed with fiber, ground flaxseeds providing fiber and healthy fats, chia seeds that add bulk to stool, pears and apples with skin, sweet potatoes, avocados, whole grains like oatmeal, and yogurt or kefir with probiotics. Focus on high-fiber, nutrient-dense foods even when eating less overall.
When should I see a doctor for Ozempic constipation?
Seek immediate medical attention if you experience severe or worsening abdominal pain, complete inability to pass stool or gas (possible bowel obstruction), vomiting along with constipation, blood in stool, fever with constipation, or severe abdominal distension. Contact your provider if constipation persists despite aggressive treatment for more than 7 to 10 days, you need stimulant laxatives regularly to have bowel movements, or over-the-counter treatments aren’t providing adequate relief.
Is it normal to only poop every few days on Ozempic?
Having bowel movements every 2 to 3 days can be normal on Ozempic if the stools remain soft and easy to pass without straining or discomfort. You’re eating significantly less food, so producing less waste is expected. However, if you’re going 4+ days without bowel movements, experiencing hard stools requiring straining, feeling bloated and uncomfortable, or experiencing abdominal pain, this indicates constipation requiring intervention.
Can Ozempic cause severe constipation?
Yes, though severe constipation is less common than mild to moderate cases. Some people develop significant constipation with hard, difficult-to-pass stools, going 5+ days without bowel movements, severe bloating and abdominal discomfort, and requiring multiple interventions for relief. Severe cases may require prescription medications or medical evaluation. If over-the-counter strategies aren’t providing adequate relief, discuss more aggressive management options with your healthcare provider.
Managing Constipation Successfully on Ozempic
Constipation is one of the more common Ozempic side effects, but it’s usually manageable with a proactive, systematic approach combining prevention and treatment strategies. Understanding that constipation results from slowed gut motility, reduced food intake, and decreased fiber consumption helps you address it effectively through aggressive hydration, prioritizing fiber intake, maintaining physical activity, and using safe, effective treatments like polyethylene glycol when needed.
For most people, constipation improves substantially within 2 to 4 weeks at each dose level as the digestive system adapts. The key to success involves starting prevention strategies from day one rather than waiting for problems to develop, using polyethylene glycol regularly to maintain comfortable bowel function when needed, avoiding dependency on stimulant laxatives, staying extremely well hydrated, and communicating with your healthcare provider if standard approaches aren’t providing adequate relief.
While constipation can be uncomfortable and frustrating, it rarely necessitates stopping treatment. The health benefits of significant weight loss typically outweigh the temporary or manageable inconvenience of addressing this side effect. Most people find that with the right combination of strategies, they can maintain comfortable bowel function while achieving their weight loss goals.
Whether you’re using brand-name Ozempic or more affordable compounded semaglutide at $199 monthly through TrimRx, understanding and managing constipation effectively allows you to pursue weight loss without letting this side effect derail your progress. Get started with comprehensive medical support and guidance on managing all aspects of treatment, including proven strategies for preventing and relieving constipation throughout your journey.

Transforming Lives, One Step at a Time
Keep reading
Online Ozempic Prescription Texas
You can get an Ozempic prescription online in Texas through a licensed telehealth provider without an in-person visit. Texas telehealth law allows providers to…
Online Ozempic Prescription California
You can get an Ozempic prescription online in California through a licensed telehealth provider without an in-person visit. California’s telehealth laws allow providers to…
Weight Loss Clinic Online Texas: Your Options
An online weight loss clinic in Texas gives you access to GLP-1 medications like semaglutide and tirzepatide through a fully virtual process. You complete…



