GLP-1 for Type 2 Diabetes: Beyond Blood Sugar Control

When GLP-1 medications first emerged for Type 2 diabetes, they were one option among many for lowering blood sugar. Today, they’ve become the cornerstone of modern diabetes treatment, and not just because they control glucose effectively. These medications have fundamentally changed what we expect from diabetes treatment by delivering benefits that extend far beyond HbA1c numbers.
The transformation in thinking happened as clinical trial data accumulated. GLP-1 agonists don’t just lower blood sugar; they produce substantial weight loss, reduce cardiovascular events, protect kidneys, and improve fatty liver disease. For many patients with Type 2 diabetes, these medications address the condition as the metabolic syndrome it actually is, rather than simply treating an elevated number.
This shift matters practically. If you have Type 2 diabetes, your medication choices affect not just your glucose readings but your weight trajectory, your heart attack risk, and your long-term organ health. Understanding what GLP-1 medications offer across all these dimensions helps you have informed conversations with your healthcare provider about optimizing your treatment.
This guide covers:
- How GLP-1 medications work and why their effects extend beyond glucose
- Blood sugar control: what results to expect
- Weight loss: magnitude and timeline
- Cardiovascular benefits: the evidence and what it means
- Kidney and liver protection
- Comparing different GLP-1 medications (semaglutide, tirzepatide, liraglutide, dulaglutide)
- How GLP-1s fit with other diabetes treatments
- Who benefits most from these medications
- Practical considerations for access and cost
Key Takeaways
- GLP-1 medications produce comprehensive metabolic improvement, addressing blood sugar, weight, cardiovascular risk, and organ health simultaneously
- HbA1c reductions average 1.0-2.0 percentage points, with many patients achieving target levels under 7%
- Weight loss averages 10-15% with semaglutide, substantially more than older diabetes medications
- Cardiovascular event reduction of 20% has been demonstrated in high-risk patients, making GLP-1s the preferred choice for patients with heart disease
- Kidney protection extends beyond what glucose control alone would provide
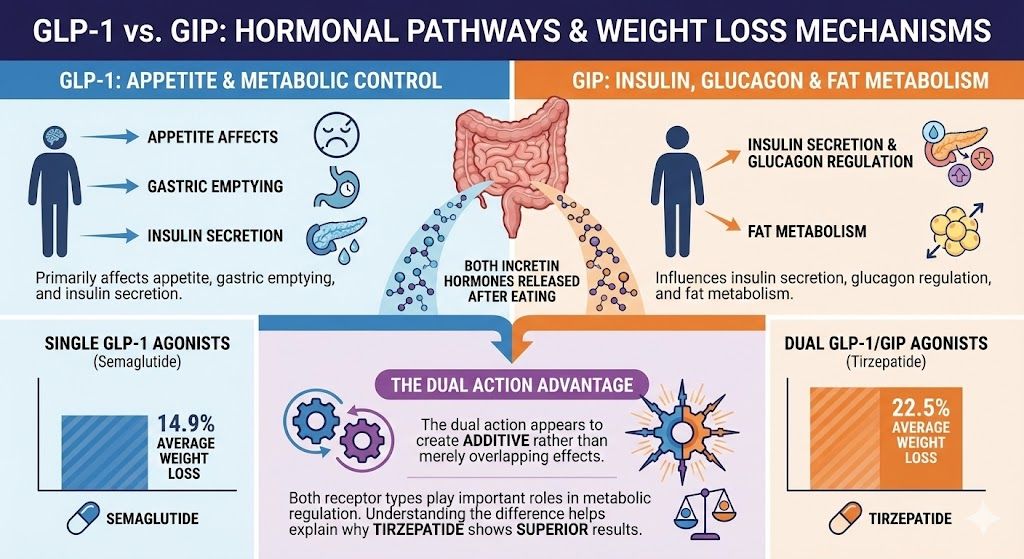
- Tirzepatide (dual GLP-1/GIP agonist) produces greater improvements than single-mechanism GLP-1 agonists
- These medications can reduce or eliminate the need for other diabetes drugs, including insulin in many cases
- Side effects are primarily gastrointestinal and usually improve with time and proper titration
- Cost remains a barrier, though compounded options and manufacturer programs improve access
- GLP-1 medications are now recommended as first-line treatment for many Type 2 diabetes patients, particularly those with cardiovascular disease or obesity
Understanding GLP-1 Medications
Before exploring their benefits, understanding how these medications work explains why they affect so many aspects of metabolic health.
What GLP-1 Is
GLP-1 (glucagon-like peptide-1) is a hormone naturally produced in your gut after eating. It’s part of the “incretin” system that helps regulate blood sugar and metabolism. Natural GLP-1 has several effects:
Insulin stimulation: GLP-1 signals the pancreas to release insulin, but only when blood sugar is elevated. This glucose-dependent action means it helps lower high blood sugar without causing dangerous drops when blood sugar is normal.
Glucagon suppression: GLP-1 reduces the release of glucagon, a hormone that tells the liver to release stored glucose. Suppressing glucagon helps prevent blood sugar from rising too high.
Appetite regulation: GLP-1 acts on brain regions controlling hunger and satiety, reducing appetite and promoting feelings of fullness.
Gastric slowing: GLP-1 slows how quickly food leaves your stomach, reducing post-meal glucose spikes and prolonging satiety.
Natural GLP-1 is broken down within minutes by an enzyme called DPP-4. GLP-1 medications are modified versions that resist this breakdown, allowing them to remain active for days rather than minutes.
GLP-1 Receptor Agonists Available
Several GLP-1 medications are available, with important differences:
| Medication | Brand Names | Dosing | Relative Potency |
| Semaglutide | Ozempic, Wegovy, Rybelsus | Weekly injection or daily oral | High |
| Tirzepatide | Mounjaro, Zepbound | Weekly injection | Highest (dual mechanism) |
| Liraglutide | Victoza, Saxenda | Daily injection | Moderate |
| Dulaglutide | Trulicity | Weekly injection | Moderate |
| Exenatide | Byetta, Bydureon | Twice daily or weekly | Lower |
Semaglutide (Ozempic for diabetes, Wegovy for weight loss) has become the most widely used due to its combination of efficacy, once-weekly dosing, and substantial clinical trial data.
Tirzepatide (Mounjaro for diabetes, Zepbound for weight loss) is the newest and most potent option. It’s technically a “dual agonist” that activates both GLP-1 and GIP (glucose-dependent insulinotropic polypeptide) receptors, producing greater effects than GLP-1-only medications.
Why Effects Extend Beyond Blood Sugar
The broad benefits of GLP-1 medications stem from addressing underlying metabolic dysfunction rather than just treating elevated glucose:
Weight loss addresses root causes: Excess weight drives insulin resistance, the core problem in Type 2 diabetes. By producing substantial weight loss, GLP-1 medications improve the fundamental metabolic dysfunction.
Systemic hormone effects: GLP-1 receptors exist throughout the body, including in the heart, blood vessels, kidneys, and liver. Activating these receptors produces direct protective effects.
Reduced metabolic stress: Lower weight, improved insulin sensitivity, and better glucose control reduce the metabolic burden on organs that are damaged by diabetes.
Anti-inflammatory effects: Some research suggests GLP-1 medications reduce chronic inflammation, which contributes to cardiovascular disease and other complications.
This comprehensive mechanism explains why GLP-1 medications have proven beneficial across multiple organ systems, not just for glucose control.
Blood Sugar Control: The Primary Indication
While this guide focuses on benefits beyond glucose, blood sugar control remains important and is where GLP-1 medications excel.
HbA1c Reductions
GLP-1 medications produce substantial reductions in HbA1c (the measure of average blood sugar over 2-3 months):
Semaglutide: Average HbA1c reduction of 1.5-1.8 percentage points in clinical trials. Patients starting at 8.5% often reach 6.7-7.0%, potentially achieving target levels.
Tirzepatide: Even greater reductions, averaging 2.0-2.3 percentage points. Some trials show average HbA1c below 6.0% with treatment.
Liraglutide: Average reduction of 1.0-1.3 percentage points.
Dulaglutide: Average reduction of 1.1-1.4 percentage points.
For context, metformin (the traditional first-line medication) typically produces 0.5-1.0 percentage point reductions. GLP-1 medications are substantially more effective for glucose control.
Fasting and Post-Meal Glucose
Beyond HbA1c, GLP-1 medications improve specific glucose patterns:
Fasting glucose: Typically decreases by 25-50 mg/dL, addressing the elevated morning blood sugar common in diabetes.
Post-meal glucose: The combination of enhanced insulin release, suppressed glucagon, and slowed gastric emptying substantially reduces glucose spikes after eating.
Glucose variability: Many patients experience more stable blood sugar with fewer highs and lows, which may independently reduce complication risk.
Comparison to Other Diabetes Medications
How do GLP-1 medications compare to other options for glucose control?
| Medication Class | HbA1c Reduction | Weight Effect | Hypoglycemia Risk |
| GLP-1 agonists | 1.0-2.0% | Weight loss | Low |
| Tirzepatide | 2.0-2.3% | Greater weight loss | Low |
| Metformin | 0.5-1.0% | Neutral/slight loss | Very low |
| SGLT2 inhibitors | 0.5-1.0% | Modest weight loss | Low |
| Sulfonylureas | 1.0-1.5% | Weight gain | Moderate |
| DPP-4 inhibitors | 0.5-0.8% | Neutral | Low |
| Insulin | Variable (potent) | Weight gain | High |
GLP-1 medications offer the unusual combination of potent glucose lowering with weight loss and low hypoglycemia risk, explaining their rising prominence.
Weight Loss: A Transformative Benefit
For many patients with Type 2 diabetes, weight loss is as important as glucose control.
Magnitude of Weight Loss
GLP-1 medications produce substantially more weight loss than older diabetes treatments:
Semaglutide (diabetes doses): Average weight loss of 10-12% of body weight at the 1mg and 2mg doses used for diabetes.
Semaglutide (weight loss doses): At the 2.4mg dose (Wegovy), average loss reaches approximately 15%.
Tirzepatide: Even greater, with average weight loss of 15-22% depending on dose.
Liraglutide: More modest at 5-8% average weight loss.
Dulaglutide: Similar to liraglutide at 3-5% average.
For a patient weighing 220 pounds, semaglutide might produce 22-33 pounds of weight loss, while tirzepatide might achieve 33-48 pounds. This magnitude of loss was previously achievable only through surgery.
Why Weight Loss Matters for Diabetes
Weight loss in diabetic patients produces benefits that extend far beyond the scale:
Improved insulin sensitivity: Each 5% of body weight lost meaningfully improves how cells respond to insulin. Significant weight loss can substantially reduce or eliminate insulin resistance.
Reduced medication needs: Many patients reduce doses or eliminate other diabetes medications as weight decreases. Some patients who required insulin achieve good control without it.
Better glucose control: Weight loss amplifies the direct glucose-lowering effects of GLP-1 medications.
Addressing root causes: Unlike medications that simply lower blood sugar, weight loss addresses the excess weight that contributed to developing diabetes in the first place.
Potential remission: Some patients who lose substantial weight achieve HbA1c below diabetic thresholds, sometimes called “remission.” While this typically requires ongoing treatment, it represents meaningful disease modification.
Weight Loss Timeline
Weight loss with GLP-1 medications follows a predictable pattern:
Months 1-2: Initial weight loss begins, typically 3-8 pounds as appetite decreases during dose titration.
Months 3-6: Weight loss accelerates at maintenance doses, with most rapid progress during this phase.
Months 6-12: Continued weight loss, though rate gradually slows.
Months 12-18: Maximum weight loss typically achieved, transitioning to maintenance.
For detailed month-by-month expectations, see our guide on Ozempic weight loss results.
Contrast With Traditional Diabetes Medications
The weight effects of GLP-1 medications contrast sharply with older diabetes treatments:
Insulin: Typically causes weight gain of 4-8 pounds over the first year, sometimes more. This creates a frustrating cycle where treating diabetes worsens one of its underlying causes.
Sulfonylureas (glipizide, glyburide): Commonly cause weight gain of 3-5 pounds.
Thiazolidinediones (pioglitazone): Often cause significant weight gain plus fluid retention.
For patients struggling with weight, the difference between a medication that produces 15% weight loss versus one causing weight gain is transformative.
Cardiovascular Benefits: Protecting the Heart
Perhaps the most important discovery about GLP-1 medications is their ability to reduce cardiovascular events, the leading cause of death in people with Type 2 diabetes.
The Evidence
Multiple large cardiovascular outcome trials have demonstrated GLP-1 medications reduce heart attacks, strokes, and cardiovascular death:
SUSTAIN-6 (semaglutide): 26% reduction in major adverse cardiovascular events (MACE) in patients with Type 2 diabetes and high cardiovascular risk.
LEADER (liraglutide): 13% reduction in MACE plus cardiovascular death reduction.
REWIND (dulaglutide): 12% reduction in MACE in a broader diabetic population.
SELECT (semaglutide): 20% reduction in MACE in patients with obesity and established cardiovascular disease (regardless of diabetes status).
SURPASS-CVOT (tirzepatide): Ongoing trial expected to demonstrate cardiovascular benefits; preliminary data is promising.
These results represent genuine reductions in heart attacks, strokes, and deaths, not just improvements in surrogate markers like cholesterol numbers.
What This Means Practically
For patients with Type 2 diabetes, these findings have practical implications:
First-line treatment recommendation: Major diabetes guidelines now recommend GLP-1 agonists as first-line treatment (alongside or instead of metformin) for patients with established cardiovascular disease.
Risk reduction beyond glucose: The cardiovascular benefits appear to exceed what glucose control alone would provide. Something about these medications directly protects the heart and blood vessels.
Medication prioritization: For diabetic patients with heart disease, GLP-1 medications should generally be prioritized over other diabetes drugs that lack cardiovascular outcome benefit.
Who Benefits Most
Cardiovascular benefits are clearest in high-risk patients:
Established cardiovascular disease: Patients with prior heart attack, stroke, or documented atherosclerosis have the strongest evidence for benefit.
High cardiovascular risk: Patients with multiple risk factors (diabetes, hypertension, high cholesterol, smoking history, family history) likely benefit, though direct trial evidence in lower-risk populations is less extensive.
Obesity with cardiovascular disease: The SELECT trial showed benefit in patients with obesity and heart disease regardless of diabetes status, expanding the population who clearly benefit.
Mechanisms of Cardiovascular Protection
How do GLP-1 medications protect the heart? Multiple mechanisms likely contribute:
Weight loss: Reduces cardiac workload, improves blood pressure, and improves lipid profiles.
Blood pressure reduction: GLP-1 medications typically reduce systolic blood pressure by 4-6 mmHg.
Improved lipid profile: Triglycerides decrease; LDL cholesterol may decrease modestly.
Reduced inflammation: Inflammatory markers often decrease, potentially reducing vascular inflammation that contributes to atherosclerosis.
Direct vascular effects: GLP-1 receptors in blood vessels may mediate direct protective effects independent of metabolic improvements.
Reduced atherogenesis: Some research suggests GLP-1 medications may slow the development of arterial plaques.
The cardiovascular benefits appear to be a class effect, with all GLP-1 agonists showing benefit, though the magnitude varies between specific medications.
Kidney Protection
Type 2 diabetes is the leading cause of kidney failure. GLP-1 medications appear to provide kidney protection beyond what glucose control alone achieves.
Evidence for Kidney Benefits
Clinical trials show consistent kidney benefits:
FLOW trial (semaglutide): This dedicated kidney outcome trial showed semaglutide reduced the risk of major kidney outcomes (kidney failure, significant decline in kidney function, or kidney-related death) by 24% in diabetic patients with chronic kidney disease. The trial was stopped early because benefits were so clear.
Kidney outcomes in cardiovascular trials: Analyses from SUSTAIN-6, LEADER, and other trials consistently show reductions in kidney-related outcomes with GLP-1 treatment.
Specific Kidney Effects
GLP-1 medications produce several kidney-relevant improvements:
Reduced albuminuria: The amount of albumin (protein) in urine, an early marker of kidney damage, typically decreases with GLP-1 treatment.
Preserved kidney function: The rate of decline in estimated glomerular filtration rate (eGFR, a measure of kidney function) is slowed.
Reduced progression to kidney failure: Fewer patients progress to dialysis or transplant.
Implications for Treatment Decisions
For diabetic patients with kidney disease or elevated risk:
Consider GLP-1 medications early: Rather than waiting for kidney disease to progress, starting GLP-1 treatment may help preserve kidney function.
Dosing considerations: Most GLP-1 medications don’t require dose adjustment for mild-to-moderate kidney impairment, though severe impairment may affect some options.
Combination potential: GLP-1 medications can be combined with SGLT2 inhibitors (another class with kidney benefits) for potentially additive protection.
Liver Benefits
Non-alcoholic fatty liver disease (NAFLD) and its more severe form, non-alcoholic steatohepatitis (NASH), affect a large proportion of patients with Type 2 diabetes. GLP-1 medications show substantial benefit.
The NAFLD-Diabetes Connection
The overlap between fatty liver disease and diabetes is significant:
Prevalence: An estimated 70% of patients with Type 2 diabetes have some degree of fatty liver disease.
Shared pathophysiology: Insulin resistance drives both conditions. Excess fat storage in the liver worsens metabolic dysfunction, creating a vicious cycle.
Progression risk: NAFLD can progress to NASH (with inflammation), fibrosis, cirrhosis, and liver failure.
Evidence for Liver Benefits
GLP-1 medications produce meaningful liver improvements:
Reduced liver fat: Studies using imaging show significant reductions in liver fat content with semaglutide and other GLP-1 medications.
Improved liver enzymes: ALT and AST (markers of liver inflammation) typically decrease with treatment.
NASH resolution: In trials specifically examining liver outcomes, a significant proportion of patients achieved resolution of NASH (the inflammatory form of fatty liver disease).
Fibrosis stabilization: Some evidence suggests GLP-1 medications may slow the progression of liver fibrosis, though they don’t appear to reverse established fibrosis.
Clinical Implications
For diabetic patients with fatty liver disease:
Dual benefit: GLP-1 medications address both conditions simultaneously.
Monitoring: Liver enzymes should be checked periodically to assess response.
Weight loss mechanism: Much of the liver benefit likely comes through weight loss, which is highly effective for fatty liver disease.
Comparing GLP-1 Medications
Not all GLP-1 medications are equal. Understanding differences helps optimize treatment selection.
Semaglutide (Ozempic, Wegovy, Rybelsus)
Strengths:
- Strong evidence base with extensive clinical trial data
- Once-weekly dosing (injection) or daily (oral)
- Excellent glucose control and weight loss
- Proven cardiovascular and kidney benefits
- Widely available
Considerations:
- Gastrointestinal side effects common initially
- Cost without insurance is significant
Best for: Most patients seeking strong glucose control with weight loss; patients with cardiovascular disease; patients preferring weekly dosing.
Tirzepatide (Mounjaro, Zepbound)
Strengths:
- Highest efficacy for both glucose control and weight loss
- Dual mechanism (GLP-1 + GIP) may provide unique benefits
- Once-weekly dosing
- Generally well-tolerated
Considerations:
- Higher cost than semaglutide
- Less long-term safety data (newer medication)
- Cardiovascular outcome trial not yet complete (though expected to be positive)
Best for: Patients prioritizing maximum weight loss; patients inadequately controlled on other GLP-1 medications; those who can manage higher cost.
For detailed comparison, see our guide on Mounjaro weight loss results.
Liraglutide (Victoza, Saxenda)
Strengths:
- Long safety track record
- Proven cardiovascular benefits
- Available in both diabetes (Victoza) and weight management (Saxenda) formulations
Considerations:
- Daily injection required
- Less weight loss than semaglutide or tirzepatide
- Less potent glucose control
Best for: Patients who prefer a longer-established medication; those who tolerate daily injections; patients with cost constraints where liraglutide is more accessible.
Dulaglutide (Trulicity)
Strengths:
- Once-weekly dosing
- Easy-to-use auto-injector device
- Proven cardiovascular benefit
- Good tolerability profile
Considerations:
- Less weight loss than semaglutide
- Moderate (not maximum) glucose efficacy
Best for: Patients prioritizing convenience and tolerability over maximum efficacy; those with cardiovascular risk wanting proven protection.
Oral Semaglutide (Rybelsus)
Strengths:
- Pill form (no injections)
- Same active medication as Ozempic
Considerations:
- Must be taken on empty stomach with minimal water
- Strict administration requirements
- Less effective than injectable semaglutide at available doses
- Daily dosing
Best for: Patients who refuse injections; those prioritizing oral administration despite reduced convenience and efficacy.
GLP-1 Medications in Diabetes Treatment Plans
Understanding how GLP-1 medications fit with other treatments helps optimize your overall diabetes management.
As First-Line Treatment
Guidelines increasingly support GLP-1 agonists as first-line treatment alongside or instead of metformin:
When to consider first-line GLP-1:
- Established cardiovascular disease
- High cardiovascular risk
- Significant obesity (BMI 35+)
- Strong desire for weight loss
- Insurance coverage available
Traditional metformin-first approach:
- Lower cost without insurance
- Decades of safety data
- Effective for many patients
- Can add GLP-1 later if needed
For many patients, starting with a GLP-1 medication rather than metformin provides superior comprehensive benefit.
Combining With Other Medications
GLP-1 medications can be combined with other diabetes drugs:
Metformin + GLP-1: Common and effective combination. Complementary mechanisms, generally well-tolerated.
SGLT2 inhibitors + GLP-1: Increasingly popular combination with complementary benefits (cardiovascular, kidney protection, weight loss). The medications work through different mechanisms and can be additive.
Insulin + GLP-1: Can be combined, often allowing significant insulin dose reduction. Some fixed-ratio combinations are available (e.g., Soliqua, Xultophy).
Sulfonylureas + GLP-1: Possible but requires caution due to increased hypoglycemia risk. Often the sulfonylurea is reduced or discontinued when adding GLP-1.
DPP-4 inhibitors: Generally discontinued when starting GLP-1 since both affect the incretin system.
Reducing Other Medications
A significant benefit of GLP-1 treatment is often simplifying medication regimens:
Insulin reduction or discontinuation: Many patients on insulin reduce doses substantially, sometimes discontinuing insulin entirely.
Sulfonylurea discontinuation: Often possible and reduces hypoglycemia risk.
Metformin continuation or discontinuation: Some providers continue metformin for its modest additional benefit and low cost; others discontinue if GLP-1 provides adequate control.
Blood pressure medications: May be reduced as blood pressure improves with weight loss.
The goal is achieving excellent metabolic control with the simplest, safest regimen possible.
Who Benefits Most From GLP-1 Medications
While GLP-1 medications benefit most patients with Type 2 diabetes, certain groups see particularly significant advantages.
Ideal Candidates
Diabetes with obesity: Patients who need both glucose control and significant weight loss are ideal candidates. GLP-1 medications address both simultaneously.
Established cardiovascular disease: The proven cardiovascular protection makes GLP-1 medications first-choice treatment for patients with heart disease.
Kidney disease: Patients with diabetic kidney disease benefit from kidney protection, especially after the FLOW trial results.
Fatty liver disease: The combination of diabetes and NAFLD/NASH is effectively addressed by GLP-1 treatment.
Insulin users wanting to reduce doses: GLP-1 medications often allow substantial insulin reduction while improving control.
Multiple medication users seeking simplification: The efficacy of GLP-1 medications often allows discontinuing other diabetes drugs.
Patients Who May See Less Dramatic Results
Type 1 diabetes: GLP-1 medications are not appropriate as primary treatment since they require functional pancreatic beta cells.
Advanced Type 2 diabetes with severe beta cell dysfunction: Patients who have had diabetes for decades with minimal remaining insulin production may see less glucose benefit (though weight loss still occurs).
Patients unable to tolerate gastrointestinal side effects: While most patients adjust, some cannot tolerate the nausea and other GI effects.
Those with specific contraindications: Personal or family history of medullary thyroid carcinoma or MEN2 syndrome, history of pancreatitis.
Practical Considerations
Several practical factors affect GLP-1 medication use.
Side Effects and Tolerability
The most common side effects are gastrointestinal:
Nausea: Affects 20-40% of patients, usually most prominent during dose increases and improving over weeks.
Vomiting: Less common than nausea but occurs in some patients.
Diarrhea: Common, particularly during early treatment.
Constipation: Also common, sometimes alternating with diarrhea.
Decreased appetite: This is both a side effect and the intended mechanism.
Management strategies:
- Follow the gradual dose titration schedule
- Eat smaller meals
- Avoid fatty, greasy foods
- Stay hydrated
- Eat slowly and stop when satisfied
- Don’t lie down immediately after eating
Most patients find side effects improve significantly after the first month or two.
Less Common Side Effects
Injection site reactions: Usually minor redness or irritation.
Fatigue: Some patients experience tiredness, particularly initially.
Hair thinning: Can occur with rapid weight loss, usually temporary.
Gallbladder problems: Weight loss increases gallstone risk; some patients develop gallbladder issues.
Serious Risks
Rare but important:
Pancreatitis: Occurs in a small percentage of patients. Severe abdominal pain should prompt immediate medical attention.
Thyroid tumors: Animal studies showed increased thyroid tumors; human risk is uncertain but the medications are contraindicated with personal or family history of medullary thyroid carcinoma.
Severe gastrointestinal problems: Rare cases of severe gastroparesis or intestinal obstruction.
Cost and Access
Cost is a significant consideration:
Brand-name pricing:
- Ozempic/Wegovy: List price approximately $1,000/month; Novo Nordisk cash-pay program $349/month
- Mounjaro/Zepbound: List price approximately $1,000/month; Lilly cash-pay programs starting at $349-499/month
Insurance coverage:
- Generally better for diabetes indication than weight loss indication
- Prior authorization typically required
- Coverage varies widely between plans
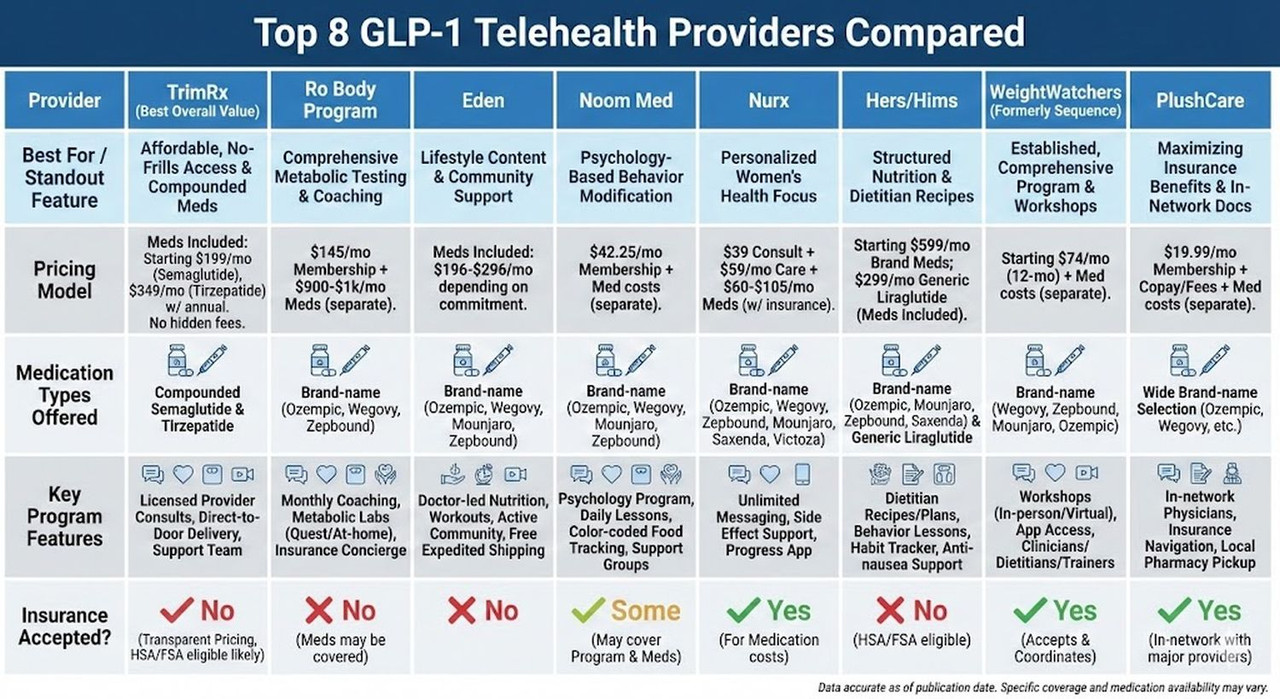
Compounded options:
- Compounded semaglutide: $199/month through TrimRx
- Compounded tirzepatide: $349/month through TrimRx
For detailed cost information, see our guides on Ozempic insurance coverage and compounded semaglutide costs.
Administration
Injectable GLP-1 medications:
- Self-administered subcutaneous injection
- Small needle, minimal discomfort for most
- Common injection sites: abdomen, thigh, upper arm
- Rotate sites to prevent tissue irritation
- Most are once-weekly (semaglutide, tirzepatide, dulaglutide)
Oral semaglutide (Rybelsus):
- Must be taken on empty stomach
- No more than 4 oz water
- Wait 30 minutes before eating or taking other medications
- Daily dosing
Long-Term Considerations
Understanding the long-term picture helps with treatment planning.
Duration of Treatment
GLP-1 medications are typically continued long-term:
Ongoing treatment: Benefits persist with continued treatment but diminish if the medication is stopped.
Weight maintenance: Research shows weight typically regains after discontinuation, suggesting ongoing treatment is needed to maintain benefits.
Metabolic maintenance: Blood sugar, cardiovascular protection, and other benefits similarly require ongoing treatment.
Planning for sustainability: Given long-term use is expected, cost sustainability matters.
What Happens If You Stop
Discontinuation typically leads to:
Weight regain: About two-thirds of lost weight typically returns within a year.
Blood sugar increase: HbA1c rises, often returning toward pre-treatment levels.
Loss of protective effects: Cardiovascular and kidney protective benefits likely diminish.
The medication manages Type 2 diabetes rather than curing it. The underlying metabolic dysfunction persists and reasserts itself without treatment.
Disease Modification Potential
While GLP-1 medications don’t cure diabetes, they may modify disease trajectory:
Preserved beta cell function: Some evidence suggests GLP-1 medications may help preserve pancreatic beta cells, potentially slowing disease progression.
Reduced complications: By improving multiple risk factors, GLP-1 treatment likely reduces the development of diabetic complications over time.
Potential remission: Some patients achieve HbA1c below diabetic thresholds. While typically requiring ongoing treatment, this represents meaningful disease modification.
Frequently Asked Questions
How do GLP-1 medications compare to insulin for Type 2 diabetes?
GLP-1 medications offer several advantages over insulin for many patients with Type 2 diabetes. They produce weight loss (versus weight gain with insulin), have lower hypoglycemia risk, and have proven cardiovascular benefits that insulin lacks. For glucose control, GLP-1 medications are often comparable to basal insulin, though high-dose insulin remains more potent for severe hyperglycemia. Many patients who start insulin can transition to GLP-1 medications or significantly reduce insulin doses when adding a GLP-1 agonist. However, insulin remains necessary for patients with Type 1 diabetes and some advanced Type 2 patients with minimal beta cell function. The choice depends on disease stage, glucose levels, weight, cardiovascular status, and other factors.
Can GLP-1 medications reverse Type 2 diabetes?
GLP-1 medications can help some patients achieve glucose levels below diabetic thresholds, sometimes called “remission.” Substantial weight loss improves insulin sensitivity, and if enough pancreatic function remains, the system may return to near-normal function. However, this typically requires ongoing treatment to maintain. If medication is stopped and weight regains, diabetes usually returns. So while the medications can produce remission-like states, they’re managing the condition rather than permanently curing it. The patients most likely to achieve remission have shorter diabetes duration, better preserved beta cell function, and achieve significant weight loss with treatment.
What makes tirzepatide different from other GLP-1 medications?
Tirzepatide is a dual agonist that activates both GLP-1 and GIP (glucose-dependent insulinotropic polypeptide) receptors, while other medications in this class activate only GLP-1 receptors. This dual mechanism produces greater effects: clinical trials show tirzepatide produces approximately 2.0-2.3 percentage point reductions in HbA1c (versus 1.5-1.8 for semaglutide) and 15-22% weight loss (versus 10-15% for semaglutide). Whether the GIP component provides unique benefits beyond simply amplifying GLP-1 effects is still being studied. Tirzepatide’s cardiovascular outcome trial is ongoing but expected to show benefit. The main tradeoff is higher cost.
Are GLP-1 medications safe for long-term use?
Current evidence suggests GLP-1 medications are safe for long-term use. Semaglutide and liraglutide have been used for years with reassuring safety profiles. The cardiovascular and kidney outcome trials involved years of follow-up and showed benefit rather than harm. The main ongoing monitoring concerns are gastrointestinal tolerability, potential thyroid tumor risk (based on animal studies; human risk remains uncertain), and gallbladder issues. Patients should report severe abdominal pain promptly. For most patients, the demonstrated benefits substantially outweigh known risks. Long-term data continues accumulating, and no significant new safety signals have emerged with broader use.
How quickly will I see results from GLP-1 medications?
Results appear at different rates for different outcomes. Appetite changes and some blood sugar improvement often occur within the first week or two. Meaningful weight loss (5+ pounds) typically takes 4-8 weeks. HbA1c, which reflects average glucose over 2-3 months, shows full treatment effect by month 3-4. Weight loss continues for 12-18 months before stabilizing. Cardiovascular benefits are demonstrated over years of follow-up and represent cumulative risk reduction. For most patients, the first 3 months provide a good indication of how well the medication is working, though weight loss continues beyond that timeframe.
Can I take GLP-1 medications with my current diabetes medications?
Usually yes, but combination requires coordination. GLP-1 medications combine safely with metformin and SGLT2 inhibitors, which have complementary mechanisms. Combination with insulin requires insulin dose reduction (often significant) to prevent hypoglycemia. Combination with sulfonylureas similarly requires dose reduction or discontinuation due to hypoglycemia risk. DPP-4 inhibitors are generally discontinued when starting GLP-1 medications since both affect the incretin system. Your provider should review all medications when starting GLP-1 treatment and make appropriate adjustments. Never adjust other diabetes medications without medical guidance.
Why do GLP-1 medications reduce cardiovascular events?
The cardiovascular benefit appears to come from multiple mechanisms. Weight loss reduces cardiac workload and improves blood pressure and lipid profiles. Blood pressure typically decreases 4-6 mmHg with GLP-1 treatment. Inflammatory markers decrease, potentially reducing vascular inflammation. GLP-1 receptors in blood vessels may mediate direct protective effects. Better glucose control reduces the metabolic stress on the cardiovascular system. The benefits exceed what would be expected from glucose control alone, suggesting direct protective effects beyond metabolic improvement. The exact mechanisms are still being studied, but the clinical benefit is clearly established in multiple large trials.
What’s the difference between Ozempic and Wegovy?
Ozempic and Wegovy both contain semaglutide and are manufactured by Novo Nordisk. The difference is FDA approval and dosing. Ozempic is approved for Type 2 diabetes at doses up to 2mg weekly. Wegovy is approved for chronic weight management at doses up to 2.4mg weekly. The medications are essentially interchangeable, though Wegovy’s slightly higher maximum dose may produce marginally greater weight loss. Insurance coverage often differs (diabetes medications are more commonly covered than weight loss medications). Compounded semaglutide provides the same active ingredient at lower cost without the brand-name distinction.
Do the benefits of GLP-1 medications last after I stop taking them?
Unfortunately, most benefits diminish after discontinuation. Weight typically regains (about two-thirds of lost weight within a year). Blood sugar rises toward pre-treatment levels. Cardiovascular and kidney protective benefits likely decrease. This pattern reflects that GLP-1 medications manage Type 2 diabetes rather than curing it. The underlying metabolic dysfunction persists and reasserts itself without treatment. For this reason, GLP-1 medications are generally considered long-term treatment rather than temporary intervention. Planning for sustained treatment, including cost sustainability, is important from the outset.
Are compounded GLP-1 medications as effective as brand-name versions?
Compounded semaglutide and tirzepatide contain the same active ingredients as brand-name medications and should produce equivalent effects. The difference is that compounded versions are prepared by compounding pharmacies rather than the original manufacturers (Novo Nordisk or Eli Lilly). Quality depends on the compounding pharmacy’s standards and processes. Reputable telehealth platforms like TrimRx partner with FDA-registered compounding pharmacies to ensure quality. Clinical experience suggests compounded versions produce equivalent results in terms of weight loss, glucose control, and other benefits. The main advantage is substantially lower cost ($199/month for compounded semaglutide versus $349+ for brand-name).
Who should not take GLP-1 medications?
GLP-1 medications are contraindicated for patients with personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2 (MEN2). History of pancreatitis is a relative contraindication. Pregnancy and breastfeeding are contraindications; women planning pregnancy should stop GLP-1 medications at least 2 months before attempting to conceive. Patients with severe gastrointestinal disease (gastroparesis, inflammatory bowel disease) may have difficulty tolerating these medications. Type 1 diabetes is not an appropriate indication. Patients should discuss their complete medical history with their provider to ensure GLP-1 treatment is appropriate.
Taking the Next Step
GLP-1 medications have transformed Type 2 diabetes treatment by delivering comprehensive metabolic improvement beyond what previous options could achieve. The combination of excellent glucose control, substantial weight loss, cardiovascular protection, and kidney benefits makes these medications the clear first choice for many patients.
Understanding what these medications offer helps you advocate for optimal treatment. If you have Type 2 diabetes with obesity, cardiovascular disease, kidney disease, or simply inadequate control on current medications, GLP-1 treatment deserves serious consideration.
The main barriers are access and cost. Working with your healthcare provider to navigate insurance coverage, or exploring compounded options for affordable access, can make these medications achievable for most patients who would benefit.
Ready to explore GLP-1 treatment options? TrimRx offers consultations with licensed providers who can evaluate your metabolic profile and prescribe compounded semaglutide at $199/month or compounded tirzepatide at $349/month for qualifying patients.

Transforming Lives, One Step at a Time
Keep reading
Ozempic Face: Causes, Prevention, and What You Need to Know
If you’ve spent any time researching Ozempic or semaglutide, you’ve probably encountered the term “Ozempic face.” Maybe you’ve seen dramatic before-and-after photos online showing…
Does Semaglutide Make You Tired? Fatigue Causes and Solutions
If you’re taking semaglutide or considering starting it, you might be wondering whether the medication will leave you feeling exhausted. Maybe you’ve heard people…
Ozempic Nausea: How to Prevent and Manage This Common Side Effect
If you’re taking Ozempic or considering starting it, the possibility of nausea probably concerns you. Maybe you’ve heard stories about people feeling queasy for…



