Ozempic for Prediabetes: Is It Right for You?

Yes, you can take Ozempic (semaglutide) for prediabetes, though it’s prescribed off-label since its FDA approval is for type 2 diabetes. More providers are prescribing semaglutide for prediabetes patients because the clinical evidence is compelling: it produces significant weight loss, improves insulin sensitivity, and dramatically reduces the risk of progressing to full type 2 diabetes. If you’ve been told your blood sugar is creeping up and lifestyle changes alone aren’t moving the needle, semaglutide is worth a serious conversation with your provider.
What Prediabetes Actually Means
Prediabetes is diagnosed when your blood sugar levels are elevated but haven’t crossed the threshold into type 2 diabetes. The specific numbers look like this:
| Marker | Normal | Prediabetes | Type 2 Diabetes |
|---|---|---|---|
| Fasting glucose | Below 100 mg/dL | 100-125 mg/dL | 126+ mg/dL |
| HbA1c | Below 5.7% | 5.7%-6.4% | 6.5%+ |
| Oral glucose tolerance | Below 140 mg/dL | 140-199 mg/dL | 200+ mg/dL |
Roughly 98 million American adults have prediabetes, and most don’t know it. The condition typically produces no symptoms, which is part of why it’s so dangerous. Without intervention, approximately 15% to 30% of people with prediabetes will develop type 2 diabetes within five years.
That progression isn’t inevitable though. Weight loss, improved insulin function, and metabolic changes can push blood sugar back into normal range. This is where semaglutide enters the picture.
How Semaglutide Works Against Prediabetes
Prediabetes is fundamentally a condition of insulin resistance and metabolic dysfunction. Your pancreas still produces insulin, but your cells aren’t responding to it efficiently. The body compensates by making more insulin, which works for a while but eventually can’t keep up. Blood sugar rises, and you’re on the path toward diabetes.
Semaglutide disrupts this progression through several mechanisms working simultaneously.
Weight reduction. Excess body fat, particularly visceral fat around the organs, is one of the primary drivers of insulin resistance. Semaglutide produces average weight loss of 14.9% of body weight in clinical trials, far exceeding what most people achieve through diet and exercise alone. For prediabetes patients, even 5% to 7% weight loss can measurably improve insulin function.
Direct insulin sensitization. Beyond weight loss, semaglutide has direct effects on how the body handles glucose. It enhances insulin secretion when blood sugar is elevated and improves how cells respond to insulin signaling. This dual action helps bring fasting glucose and post-meal glucose levels down.
Appetite and behavior changes. Semaglutide reduces hunger and cravings by acting on brain regions that control appetite. For prediabetes patients who struggle with overeating or carbohydrate-heavy diets that spike blood sugar, this neurological effect makes dietary changes feel achievable rather than punishing.
Slowed gastric emptying. Food moves through your stomach more slowly on semaglutide, which blunts post-meal blood sugar spikes. Prediabetes patients often have exaggerated glucose responses after eating. Slower digestion smooths those peaks and gives insulin more time to work.
The Research on Semaglutide and Diabetes Prevention
The evidence for semaglutide in prediabetes has moved well past theoretical. Recent analyses from major clinical programs provide concrete numbers.
Data from the STEP 1 trial population showed that among participants with prediabetes at baseline, semaglutide 2.4 mg reduced the risk of developing type 2 diabetes by 79% compared to placebo over 68 weeks. The majority of semaglutide-treated participants with prediabetes saw their blood sugar return to normal range, a result the researchers described as regression to normoglycemia.
Citation: Garvey, W.T., et al. “Semaglutide effects on the progression to type 2 diabetes among individuals with prediabetes.” Nature Medicine, 2024. PubMed
To put that 79% risk reduction in context, the landmark Diabetes Prevention Program study from the early 2000s showed that intensive lifestyle intervention reduced diabetes risk by 58% and metformin reduced it by 31%. Semaglutide appears to exceed both of these benchmarks substantially, though direct head-to-head comparisons in the same trial are still needed.
The weight loss itself accounts for a large portion of the benefit, but researchers believe semaglutide’s direct metabolic effects contribute independently. Patients who lost the same amount of weight on semaglutide showed greater improvements in glucose metabolism than would be expected from weight loss alone.
Who’s a Good Candidate
Not every prediabetes patient needs medication. For someone with an HbA1c of 5.7% who is mildly overweight and hasn’t yet tried serious lifestyle modifications, starting with diet, exercise, and behavioral changes makes sense. Medication can always be added later if those approaches fall short.
Semaglutide becomes a stronger consideration when certain factors are present:
BMI of 27 or higher with prediabetes. The combination of excess weight and insulin resistance creates a compounding risk. Semaglutide addresses both simultaneously, which is its key advantage over interventions that target only one factor.
HbA1c trending upward. If your HbA1c has been climbing over successive lab draws, say from 5.8% to 6.1% to 6.3%, that trajectory suggests lifestyle changes alone aren’t enough. Intervening pharmacologically before reaching 6.5% is proactive, not premature.
Prior attempts at weight loss haven’t worked. Let’s say a patient has tried structured dieting, increased physical activity, and maybe even metformin, but their weight hasn’t budged and their blood sugar keeps rising. At that point, semaglutide offers a different mechanism that may succeed where other approaches stalled.
Family history of type 2 diabetes. Genetic predisposition to diabetes raises the stakes. If your parents or siblings developed type 2 diabetes, your prediabetes carries a higher likelihood of progression, making earlier pharmacological intervention more reasonable.
Metabolic syndrome features. If prediabetes comes alongside high triglycerides, low HDL cholesterol, elevated blood pressure, and central obesity, you’re dealing with metabolic syndrome. Semaglutide can improve multiple components of this cluster simultaneously.
What Results Look Like for Prediabetes Patients
The timeline of improvement on semaglutide follows a fairly predictable pattern for prediabetes patients, though individual variation is normal.
Month 1: Appetite suppression begins within the first week of semaglutide for most patients. Weight loss starts, typically 3 to 5 pounds in the first month. Blood sugar changes are subtle at this early stage, though some patients notice fewer post-meal energy crashes.
Months 2 to 3: Weight loss accelerates as the dose increases. Patients on a steady escalation schedule often see 5% to 8% total body weight loss by month three. Fasting glucose levels may begin dropping, and if you’re checking blood sugar at home, the trend becomes visible.
Months 3 to 6: This is where the metabolic improvements become measurable on lab work. HbA1c typically drops by 0.3% to 0.8% from baseline, depending on starting values and weight lost. Fasting insulin levels decline as insulin sensitivity improves. Many patients cross back from prediabetes into normal glycemic range during this window.
Months 6 to 12: Continued weight loss and sustained metabolic improvement. Patients who reach 10% to 15% total body weight loss often see their HbA1c return fully to normal range (below 5.7%) and stay there. Cardiovascular risk markers like triglycerides and blood pressure also tend to improve.
These results depend on consistent medication use, and research shows that stopping semaglutide can lead to weight regain and metabolic backsliding. The question of how long to continue treatment is one to discuss with your provider based on your progress and risk profile.
Semaglutide vs. Metformin for Prediabetes
Metformin has been the standard pharmacological tool for prediabetes prevention for over two decades. It’s cheap, well-studied, and modestly effective. But how does it compare to semaglutide?
Weight loss: Metformin produces average weight loss of 2% to 3% of body weight. Semaglutide produces 10% to 15%. For prediabetes patients whose metabolic risk is closely tied to excess weight, that gap is enormous.
Diabetes risk reduction: Metformin reduces diabetes progression risk by roughly 31%. Semaglutide data suggests a 79% risk reduction. Again, not a close contest.
Cost: Metformin costs under $10 per month as a generic. Brand-name Ozempic costs over $1,000 monthly. Compounded semaglutide narrows that gap significantly but still costs more than metformin.
Side effects: Both medications cause gastrointestinal side effects. Metformin commonly causes diarrhea, while semaglutide more often causes nausea. Both tend to improve with time and dose adjustment.
Combination potential: These medications aren’t mutually exclusive. Some providers prescribe both, using metformin’s insulin-sensitizing effects alongside semaglutide’s weight loss and appetite control. The combination can be particularly effective for patients with significant insulin resistance.
Accessing Semaglutide for Prediabetes
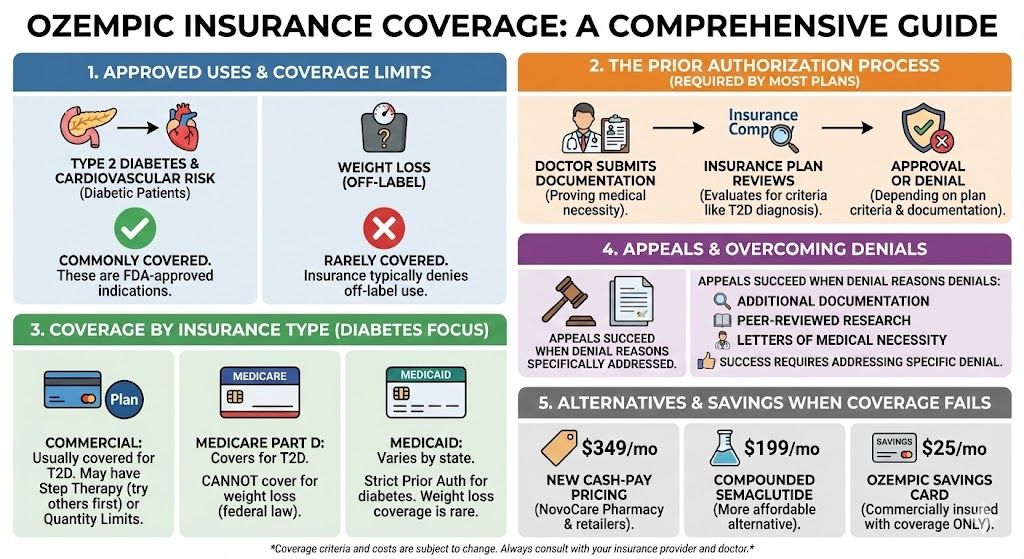
Getting insurance to cover Ozempic for prediabetes is difficult since it’s an off-label use. Most patients exploring semaglutide for prediabetes end up paying out of pocket, which is where cost becomes the deciding factor.
Compounded semaglutide through TrimRx starts at $179 per month, removing the insurance barrier entirely. For prediabetes patients, this means you can start treatment based on clinical need rather than waiting for an insurance approval that may never come.
The math of prevention is straightforward. Spending $179 per month now to reverse prediabetes and avoid type 2 diabetes is far less expensive than managing diabetes for decades with medications, monitoring supplies, specialist visits, and potential complications. It’s also far less expensive than brand-name Ozempic’s cash price.
Is Semaglutide Right for Your Prediabetes?
If your blood sugar is trending in the wrong direction, you carry excess weight, and lifestyle changes haven’t been enough on their own, semaglutide is one of the most effective tools available. The research supports it. The clinical experience supports it. The remaining question is finding an affordable, accessible way to start.
TrimRx’s online intake quiz takes just a few minutes and connects you with a licensed provider who can evaluate whether semaglutide fits your situation. No insurance paperwork, no prior authorization delays.
This information is for educational purposes and is not medical advice. Consult with a healthcare provider before starting any medication. Individual results may vary.

Transforming Lives, One Step at a Time
Keep reading
Will Insurance Cover Ozempic for Prediabetes?
In most cases, insurance will not cover Ozempic for prediabetes. Ozempic (semaglutide) is FDA-approved specifically for type 2 diabetes, not prediabetes. Since insurance companies…
Ozempic for PCOS: What the Research Shows
Research increasingly supports semaglutide (the active ingredient in Ozempic) as an effective treatment for women with PCOS, particularly for reducing weight, improving insulin resistance,…
Ozempic and PCOS: Can It Help?
Ozempic (semaglutide) isn’t FDA-approved for PCOS, but growing research and clinical experience suggest it can meaningfully help women with polycystic ovary syndrome, particularly when…



