How Long Can You Stay on Ozempic? Long-Term Use Guidelines

One of the most common questions about Ozempic is how long you can take it. If it’s working well, do you take it forever? Is there a maximum duration? What happens to your body after years of use? These questions are reasonable and important for anyone considering or currently using the medication.
The straightforward answer: There is no maximum duration for Ozempic use. The medication is approved for chronic, long-term treatment with no predetermined stopping point. Clinical trials have studied semaglutide for up to four years with continued safety and efficacy, and many patients have now used it even longer in real-world practice. From a medical standpoint, you can stay on Ozempic indefinitely as long as it remains beneficial and you tolerate it well.
However, “can” and “should” are different questions. The decision to continue long-term involves weighing ongoing benefits against costs, considering whether you’ve achieved sustainable lifestyle changes, and understanding what happens if you stop. For most patients, obesity and Type 2 diabetes are chronic conditions that benefit from ongoing management, much like high blood pressure or high cholesterol. Stopping medication typically leads to weight regain and worsening of the conditions being treated.
This guide covers:
- Official guidelines on treatment duration
- Long-term safety data (what we know so far)
- What happens when you stop taking Ozempic
- Whether benefits are maintained with continued use
- When stopping might be appropriate
- Managing treatment over years
- Long-term side effect considerations
- Cost and practical aspects of indefinite use
- How to discuss duration with your healthcare provider
Key Takeaways
- No maximum duration exists for Ozempic use; it’s approved for chronic, indefinite treatment
- Clinical trials have studied semaglutide for up to four years with sustained safety and efficacy
- Stopping typically leads to weight regain: Research shows approximately two-thirds of lost weight returns within one year of discontinuation
- Benefits are maintained with continued use; the medication continues working as long as you take it
- Long-term safety data is reassuring with no major safety signals emerging in extended studies
- Obesity is a chronic condition that typically requires ongoing management, similar to hypertension or diabetes
- Some patients may successfully stop after achieving goals and making sustainable lifestyle changes, but this is not typical
- Dose adjustments may be possible over time, with some patients maintaining results on lower doses
- Regular monitoring helps ensure ongoing safety and benefit
- Cost is a practical consideration since treatment is typically lifelong
Official Guidelines on Duration
Medical guidelines and FDA labeling provide the framework for understanding treatment duration.
FDA Approval Language
Ozempic (diabetes indication):
- Approved as “adjunct to diet and exercise”
- No maximum treatment duration specified
- Intended for chronic disease management
Wegovy (weight management indication):
- Approved for “chronic weight management”
- The word “chronic” indicates ongoing, not time-limited treatment
- No stopping point defined in labeling
What “chronic” means: In medical terminology, “chronic” refers to long-lasting conditions requiring ongoing management. Chronic treatment is designed to continue as long as the condition persists and the medication provides benefit.
Clinical Practice Guidelines
American Diabetes Association (ADA):
- Recommends GLP-1 agonists as long-term therapy
- No suggested stopping point for effective treatment
- Emphasizes individualized, ongoing assessment
Obesity Medicine Association:
- Recognizes obesity as a chronic disease
- Supports long-term pharmacotherapy
- Recommends continuing treatment as long as beneficial
Endocrine Society:
- Supports chronic use of obesity medications
- Emphasizes that stopping often leads to weight regain
- Recommends ongoing treatment for chronic weight management
What the Guidelines Mean Practically
The consistent message from regulatory bodies and medical societies:
Ozempic is designed for long-term use. Unlike short-term weight loss interventions, GLP-1 medications are intended as ongoing therapy. There’s no expectation that patients will “complete” treatment and stop.
Stopping is a choice, not a requirement. Nothing in the guidelines suggests you should stop after a certain time. Discontinuation is based on individual circumstances, not arbitrary duration limits.
Long-Term Safety Data
Understanding what we know about extended use helps inform decisions about ongoing treatment.
Clinical Trial Duration
SUSTAIN trials (diabetes):
- Up to 2 years of data
- No new safety signals with extended use
- Efficacy maintained throughout
STEP trials (weight management):
- Up to 68 weeks (approximately 16 months)
- Safety profile consistent with shorter-term use
- Weight loss maintained with continued treatment
STEP 5 trial:
- Extended to 2 years
- Demonstrated sustained weight loss
- No increased safety concerns with longer duration
SELECT trial (cardiovascular outcomes):
- Median follow-up of 39.8 months (over 3 years)
- Some participants followed for up to 4+ years
- Cardiovascular protection confirmed
- No new long-term safety issues identified
Real-World Extended Use
Post-marketing experience:
- Ozempic available since 2017 (8+ years)
- Millions of patients have used it
- No major unexpected safety signals have emerged
- FDA continues to monitor through adverse event reporting
What this tells us:
- The medication has been used for years without concerning patterns emerging
- Long-term safety appears consistent with clinical trial findings
- Ongoing monitoring continues
Known Long-Term Considerations
Effects that persist:
- GI side effects may continue but often diminish over time
- Appetite suppression is maintained with continued use
- Weight loss is maintained (doesn’t reverse while on medication)
Potential long-term concerns (theoretical or under study):
- Thyroid effects: Animal studies showed thyroid tumors, but human relevance is uncertain. Ongoing monitoring has not confirmed increased human thyroid cancer.
- Gallbladder disease: Risk exists throughout treatment, not increasing over time
- Pancreatitis: Rare, not clearly time-dependent
- Muscle mass: Long-term weight loss may affect muscle; ongoing attention to protein and exercise is important
What hasn’t emerged:
- No evidence of cumulative toxicity
- No evidence of increasing side effect severity over time
- No evidence of organ damage with extended use
- No evidence of tolerance requiring ever-increasing doses
Cardiovascular Benefits Over Time
SELECT trial findings:
- Cardiovascular protection was significant even with extended use
- Benefits accumulated over time
- Longer treatment associated with continued protection
- No evidence of diminishing cardiovascular benefit
This suggests that extended use not only maintains weight loss but continues providing cardiovascular protection.
What Happens When You Stop
Understanding discontinuation effects is crucial for decision-making.
The Weight Regain Pattern
STEP 1 Extension Study:
- Patients who stopped semaglutide after 68 weeks were followed
- Within one year of stopping, approximately two-thirds of lost weight returned
- Weight continued trending upward toward baseline
What this looks like:
- Initial: 220 pounds
- After treatment: 187 pounds (33 pounds lost)
- One year after stopping: Approximately 209 pounds (22 pounds regained)
Why Weight Returns
Biological factors:
- Appetite suppression ends when medication stops
- Hunger and cravings return to previous levels
- Gastric emptying normalizes (less prolonged fullness)
- Metabolic adaptations to weight loss persist (lower calorie needs)
The “defended set point”:
- Your body has regulatory mechanisms that “defend” your previous weight
- These mechanisms don’t reset permanently with medication
- They push toward weight regain when medication stops
Behavioral reality:
- Maintaining reduced intake without appetite suppression is very difficult
- The same biological drives that caused weight gain remain
- Lifestyle changes help but often can’t fully compensate
Blood Sugar Effects
For patients with Type 2 diabetes:
- Blood sugar typically worsens after stopping
- May return to pre-treatment levels
- May require re-starting or alternative diabetes medications
For patients with prediabetes:
- Improvements may not persist
- Risk of progression to diabetes may return
Cardiovascular Protection
After stopping:
- Unclear if cardiovascular benefits persist
- Weight regain likely reduces or reverses some protection
- Blood pressure and lipid improvements may not persist
The Chronic Disease Analogy
Consider blood pressure medication:
- Stopping typically causes blood pressure to rise again
- The medication manages the condition; it doesn’t cure it
- Most people understand ongoing treatment is needed
Ozempic works similarly:
- It manages appetite and metabolism
- It doesn’t permanently change the underlying biology
- Stopping returns you to your previous biological state
This is why obesity medicine experts increasingly view weight management medication as chronic therapy for a chronic condition.
Are Benefits Maintained Long-Term?
A key question is whether the medication continues working or loses effectiveness over time.
Weight Loss Maintenance
Evidence from trials:
- Weight loss is maintained with continued treatment
- No significant rebound while continuing medication
- The medication continues suppressing appetite
What this means:
- You don’t need to keep increasing doses to maintain effect
- The initial weight loss doesn’t reverse while on medication
- Benefits persist as long as you continue treatment
Does Tolerance Develop?
Theoretical concern:
- With many medications, the body adapts and effects diminish
- This is called “tolerance” or “tachyphylaxis”
With semaglutide:
- Clinically significant tolerance does not appear to develop
- Appetite suppression persists with ongoing use
- Weight loss is maintained, not progressively reversing
- No evidence that higher doses are needed over time
Some adaptation occurs:
- GI side effects often diminish (positive adaptation)
- Some patients report slightly less appetite suppression over years
- However, this doesn’t appear to cause significant weight regain
Blood Sugar Control
Long-term glucose management:
- HbA1c improvements are maintained with continued use
- Some evidence suggests ongoing beta cell preservation
- Glucose control doesn’t deteriorate while on medication
Natural diabetes progression:
- Type 2 diabetes often progresses over time regardless of treatment
- Some patients may eventually need additional medications
- This reflects disease progression, not medication failure
Cardiovascular Protection
Ongoing benefits:
- SELECT trial showed continued protection over 3+ years
- No evidence of diminishing cardiovascular benefit
- Longer use associated with accumulated protection
When Might Stopping Be Appropriate?
While most patients benefit from ongoing treatment, some situations may warrant discontinuation.
Legitimate Reasons to Stop
Intolerable side effects:
- Persistent GI effects that don’t improve
- Side effects significantly impacting quality of life
- Other adverse effects requiring discontinuation
Medical reasons:
- Pregnancy planning (stop before conception)
- Development of contraindications (medullary thyroid cancer, etc.)
- Significant weight loss leading to underweight status
- Other medical situations where provider recommends stopping
Personal/practical reasons:
- Cost becomes unmanageable
- Decision to try managing without medication
- Personal preference after achieving goals
Successful lifestyle transformation:
- Some patients achieve sustainable lifestyle changes
- May maintain significant weight loss without medication
- This is less common but does occur
Who Might Successfully Stop
Characteristics that may predict success:
- Significant lifestyle changes established during treatment
- Relatively modest weight loss goals achieved
- Strong behavioral foundation built
- Active exercise routine maintained
- Dietary changes that feel sustainable
- No history of weight cycling before treatment
Reality check:
- Most patients regain weight after stopping
- Even with excellent lifestyle habits, biological drives are powerful
- Success without medication is possible but not typical
- Trial discontinuation can be considered with close monitoring
Trying to Stop
If considering discontinuation:
- Discuss with your healthcare provider
- Have realistic expectations (weight regain is likely)
- Consider a trial period with close monitoring
- Plan what you’ll do if weight returns
- Be willing to restart if needed
- Don’t view restarting as “failure”
Gradual versus abrupt:
- No medical need for gradual tapering
- Some patients prefer gradual reduction psychologically
- Either approach is acceptable
Long-Term Management Strategies
If you’re planning to continue Ozempic indefinitely, here’s how to optimize ongoing treatment.
Dose Optimization
Finding your maintenance dose:
- Not everyone needs the maximum dose long-term
- Some patients maintain results on 1.0mg or 1.7mg
- Higher doses mean more medication, more cost, potentially more side effects
Considering dose reduction:
- After reaching weight goals, discuss with provider
- Trial lower dose and monitor
- Return to higher dose if weight increases
- Some patients find a lower effective dose for maintenance
When higher doses are needed:
- Inadequate appetite suppression at lower doses
- Weight regain at lower doses
- Maximum dose may be necessary for some patients
Ongoing Monitoring
Regular assessments:
- Periodic check-ins with healthcare provider
- Weight monitoring
- Blood sugar monitoring if diabetic
- General health assessment
Lab work:
- Periodic metabolic panel (kidney function, etc.)
- HbA1c if diabetic
- Lipid panel
- Other tests as indicated
What to watch for:
- Changes in effectiveness
- New side effects
- Changes in overall health
- Signs of conditions requiring attention
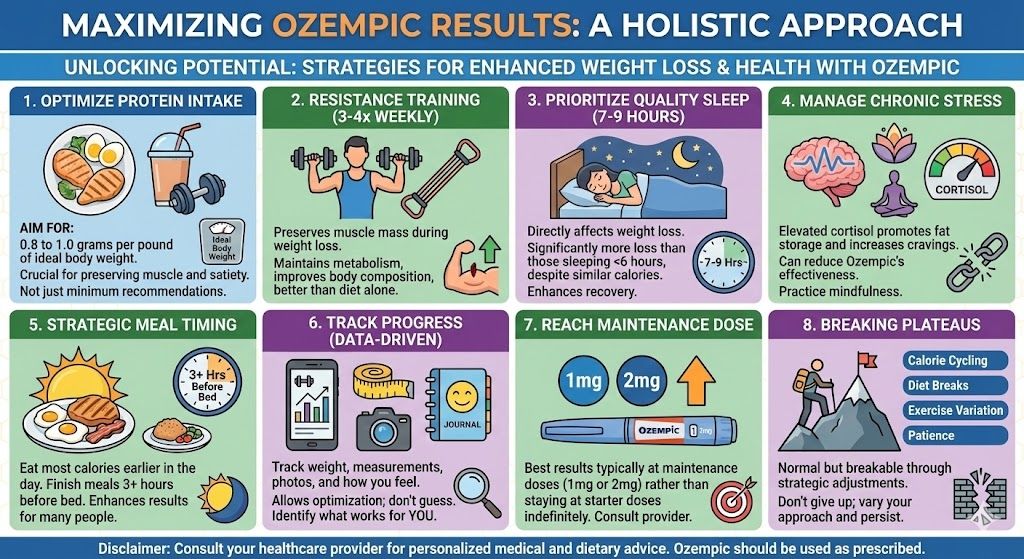
Maintaining Lifestyle Factors
Why lifestyle still matters:
- Medication works best combined with healthy habits
- Muscle preservation requires protein and exercise
- Overall health benefits from lifestyle factors
- May potentially allow lower doses
Key ongoing habits:
- Regular physical activity (especially resistance training)
- Adequate protein intake (0.8-1.0 g/kg body weight)
- Nutritious, balanced diet
- Adequate hydration
- Regular sleep
Managing Side Effects Long-Term
Persistent GI effects:
- Some patients have ongoing mild nausea
- Dietary strategies help (smaller meals, avoiding triggers)
- Usually manageable and not severe
Constipation:
- May persist throughout treatment
- Fiber, fluids, and sometimes laxatives help
- Generally manageable
Other effects:
- Report new or worsening symptoms
- Most side effects are stable or improve over time
- New symptoms warrant evaluation
Practical Considerations for Long-Term Use
Ongoing treatment has practical implications beyond medical factors.
Cost Over Time
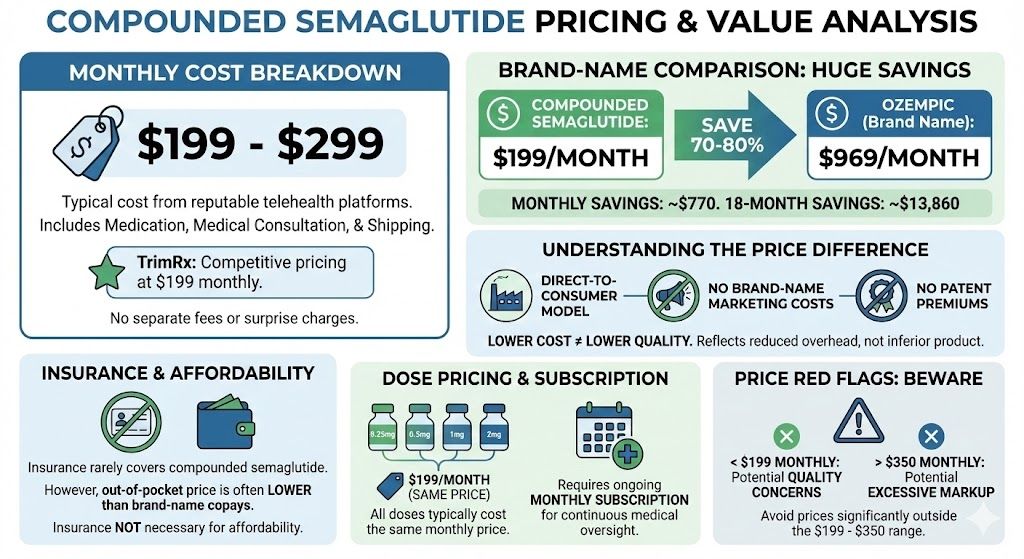
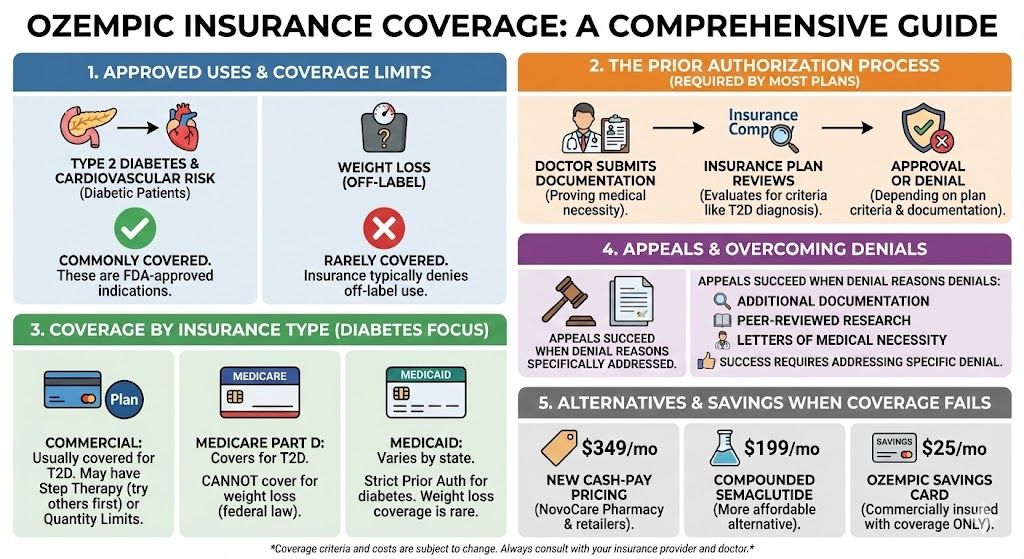
Annual costs:
- Brand-name (cash pay): ~$4,200/year (at $349/month)
- Compounded: ~$2,400/year (at $199/month)
- With insurance: Variable
Lifetime cost consideration:
- Treatment is typically indefinite
- Total cost accumulates over years/decades
- Budget planning is important
Cost management strategies:
- Explore all pricing options
- Consider compounded semaglutide
- Use manufacturer programs if eligible
- Discuss cost concerns with provider
For detailed pricing information, see our guide on compounded semaglutide costs.
Prescription Continuity
Maintaining access:
- Ongoing relationship with prescribing provider
- Regular follow-up appointments (often can be telehealth)
- Prescription renewals as needed
Avoiding gaps:
- Plan refills before running out
- Maintain appointment schedule
- Address insurance/coverage issues proactively
Travel and Lifestyle
Traveling with Ozempic:
- Plan for medication during trips
- Consider timing (weekly dosing is flexible)
- Proper storage during travel
- Ensure sufficient supply for trip duration
Lifestyle integration:
- Weekly injection becomes routine
- Minimal daily impact once established
- Flexible timing within the week
Age-Specific Considerations
Long-term use considerations may vary by age.
Younger Adults
Potentially decades of use:
- Starting in your 30s or 40s means potentially 30-50+ years
- Long-term safety data spans years, not decades
- Unknown effects of truly lifelong use
Considerations:
- Fertility planning (stop before pregnancy)
- Muscle preservation over decades
- Evolving evidence will inform care over time
Middle Age
Common treatment population:
- Many patients start in their 40s-60s
- Treatment may span 20-40 years
- Strong evidence base for this population
Focus areas:
- Cardiovascular protection (especially valuable)
- Diabetes prevention/management
- Maintaining functional capacity
Older Adults
Special considerations:
- Muscle mass preservation is critical
- Fall risk considerations
- Medication interactions
- Different risk-benefit balance
Potential advantages:
- Cardiovascular protection is valuable
- Mobility improvement from weight loss
- May allow reduction of other medications
For more on age-specific considerations, see our guide on Ozempic for seniors.
Discussing Duration With Your Provider
Having productive conversations about treatment duration helps optimize your care.
Questions to Ask
About your specific situation:
- Based on my health, do you recommend indefinite treatment?
- What would need to happen for me to consider stopping?
- How will we monitor my progress over years?
- What signs would suggest I should continue versus stop?
About adjustments over time:
- Should we try a lower dose for maintenance?
- How often should we reassess my treatment?
- What changes should prompt a conversation?
About stopping:
- If I wanted to try stopping, how would we do it?
- What should I expect if I stop?
- How would we handle weight regain?
Setting Expectations
Understand from the start:
- This is likely a long-term or lifelong treatment
- Stopping typically leads to weight regain
- The medication manages, doesn’t cure, the condition
- Ongoing treatment is the norm, not the exception
Periodic reassessment:
- Goals may evolve over time
- Circumstances change
- Regular conversations about treatment plan are appropriate
Emerging Research and Future Considerations
The field is evolving, which may affect long-term treatment approaches.
Ongoing Studies
Extended duration trials:
- Longer studies are ongoing
- Will provide more long-term safety data
- May inform optimal duration recommendations
Discontinuation research:
- Studies examining who successfully stops
- Research on strategies to maintain weight after stopping
- May eventually identify patients who can safely discontinue
Potential Future Developments
New medications:
- Next-generation GLP-1 agonists in development
- Combination therapies being studied
- May offer alternatives or additions
Different approaches:
- Intermittent dosing strategies being researched
- Combination with other interventions
- Personalized treatment protocols
What this means:
- Treatment approaches may evolve
- Staying informed and maintaining provider relationship allows adaptation
- Current guidance is based on best available evidence
Frequently Asked Questions
Is there a maximum time you can take Ozempic?
No, there is no maximum duration for Ozempic use. The medication is approved for chronic, indefinite treatment of Type 2 diabetes and (as Wegovy) for chronic weight management. Clinical trials have studied semaglutide for up to four years with continued safety and efficacy, and many patients have used it longer in real-world practice. The FDA labeling uses the word “chronic,” indicating ongoing rather than time-limited therapy. As long as the medication continues to be beneficial and you tolerate it well, you can continue taking it indefinitely.
Will Ozempic stop working after a while?
Ozempic does not appear to stop working with continued use. Clinical trials and real-world experience show that weight loss is maintained with ongoing treatment, and appetite suppression persists. Unlike some medications where tolerance develops and effectiveness diminishes, semaglutide continues working as long as you take it. Some patients report slightly less intense appetite suppression after years of use, but this typically doesn’t result in significant weight regain. The medication doesn’t require increasing doses to maintain its effect.
What happens to your body after years of taking Ozempic?
Based on available data (studies up to 4+ years), the body continues responding to Ozempic without significant adverse changes. Weight loss is maintained, blood sugar control persists, and cardiovascular protection continues. No cumulative toxicity or organ damage has been identified with extended use. GI side effects often diminish over time rather than worsening. The main consideration is maintaining muscle mass through adequate protein intake and exercise, as any long-term weight loss can affect muscle if not addressed. Long-term monitoring with your healthcare provider ensures ongoing safety.
Will I regain weight if I stop taking Ozempic?
Yes, weight regain is typical after stopping Ozempic. Research shows that within one year of discontinuation, approximately two-thirds of lost weight returns. This happens because the biological factors that originally caused weight gain (appetite regulation, hormonal signals, metabolic processes) return to their previous state when the medication stops. The medication manages these factors but doesn’t permanently change them. This is why obesity medicine experts consider GLP-1 medications as chronic therapy for a chronic condition, similar to blood pressure medication managing hypertension.
Can I take a lower dose of Ozempic for maintenance?
Some patients can maintain their results on lower doses than they used for initial weight loss. After reaching your goals, discuss with your provider whether trying a lower dose (such as 1.0mg or 1.7mg instead of 2.0mg or 2.4mg) might work for you. This can reduce cost and potentially side effects. If weight begins increasing at the lower dose, you can return to the higher dose. Not everyone can successfully reduce their dose—some patients need the maximum dose for maintenance—but it’s worth exploring with provider guidance.
Is it safe to take Ozempic for 10 or 20 years?
We don’t yet have 10 or 20-year safety data since the medication hasn’t been available that long. However, available evidence (up to 4+ years in clinical trials, 8+ years of real-world use) is reassuring with no major safety signals emerging over time. The medication works through natural GLP-1 pathways that your body already uses, which provides some theoretical reassurance. As with any long-term medication, ongoing monitoring is appropriate. The safety profile appears consistent whether used for one year or several years, and no evidence suggests safety deteriorates with extended use.
How do I know if I should continue or stop Ozempic?
Consider continuing if: the medication is effectively managing your weight or diabetes, you tolerate it reasonably well, you can afford ongoing treatment, and you haven’t developed contraindications. Consider stopping if: you experience intolerable side effects, you develop a contraindication (like pregnancy planning), cost becomes unmanageable, or you’ve made substantial lifestyle changes and want to try maintaining without medication. Discuss with your provider, who can help weigh your specific circumstances. If you do stop, monitor closely and be prepared to restart if weight regain occurs.
Do the cardiovascular benefits of Ozempic continue with long-term use?
Yes, cardiovascular benefits continue with extended use. The SELECT trial followed patients for over three years and found sustained cardiovascular protection, with a 20% reduction in major cardiovascular events. There’s no evidence that these benefits diminish over time—if anything, longer use may provide accumulated protection. This ongoing cardiovascular benefit is one important reason to consider long-term treatment, especially for patients with cardiovascular disease or significant risk factors. Stopping treatment may result in loss of this protection.
Can I take Ozempic for weight loss and then stop once I reach my goal?
You can stop at any point, but weight regain is expected. Reaching your goal weight doesn’t mean the underlying biological factors driving weight gain have changed. Without the appetite-suppressing effects of the medication, most patients gradually regain weight. Some patients do successfully maintain weight loss after stopping, particularly those who have made substantial lifestyle changes, but this is the exception rather than the rule. If you want to try stopping, do so with realistic expectations and a plan to restart if weight returns.
Should I take breaks from Ozempic?
There’s no medical reason to take periodic breaks from Ozempic. Unlike some medications where “drug holidays” serve a purpose, continuous treatment with GLP-1 medications is the standard approach. Taking breaks would likely result in temporary weight regain and then re-loss when restarting, which isn’t beneficial and could be discouraging. If you’re considering breaks due to cost, side effects, or other concerns, discuss with your provider to find better solutions than intermittent treatment.
What monitoring is needed for long-term Ozempic use?
Long-term monitoring typically includes periodic check-ins with your healthcare provider to assess weight, overall health, and any side effects. If you have diabetes, regular HbA1c monitoring continues. Periodic blood work (metabolic panel, lipids) is reasonable. Report any new symptoms, particularly severe abdominal pain (possible pancreatitis), thyroid lumps, or significant changes in how you feel. There’s no specific invasive monitoring required for long-term GLP-1 use. The monitoring schedule should be individualized based on your health status and other conditions.
The Bottom Line
There is no maximum duration for Ozempic treatment. The medication is designed and approved for chronic, indefinite use, and clinical evidence up to four years supports both safety and sustained efficacy. Most patients who benefit from Ozempic will benefit from continuing it long-term, as stopping typically results in weight regain and worsening of the conditions being treated.
This isn’t a failure of the medication or of the patient—it reflects the nature of obesity and metabolic disease as chronic conditions requiring ongoing management. Just as most patients with hypertension take blood pressure medication indefinitely, most patients with obesity benefit from long-term weight management medication.
The decision to continue, adjust, or stop treatment should be made individually with your healthcare provider, considering your specific circumstances, goals, and response to treatment. For most patients, the evidence supports ongoing treatment as long as the medication remains beneficial, tolerable, and accessible.
Ready to explore semaglutide treatment? TrimRx offers consultations with licensed providers who can evaluate your eligibility and prescribe compounded semaglutide at $199/month for qualifying patients.

Transforming Lives, One Step at a Time
Keep reading
Thyroid Issues and Ozempic: Safety Considerations
If you have a thyroid condition and you’re considering Ozempic or another GLP-1 medication for weight loss, you’ve probably come across some alarming language…
Postpartum Weight Loss: Is Ozempic Safe?
The postpartum period is one of the most physically and emotionally demanding stretches of a woman’s life, and for many new mothers, weight retained…
Ozempic While Trying to Conceive: What to Know
If you’re trying to get pregnant and also managing your weight with Ozempic, you’re navigating a genuinely complex situation. The short answer: most providers…