How Long Can You Take Semaglutide?

There is no established maximum duration for semaglutide use. Whether you’re taking brand-name Ozempic, Wegovy, or compounded semaglutide, the medication is designed for long-term, ongoing treatment. Clinical trials have studied semaglutide for weight management for up to two years with sustained efficacy and a consistent safety profile. The FDA has approved semaglutide (as Wegovy) for chronic weight management without a recommended stopping point. In clinical practice, many patients have now been on semaglutide for four or more years continuously, and the evidence consistently shows that continued use maintains results while discontinuation leads to significant weight regain.
Here’s the full picture of what long-term semaglutide use looks like, what we know and don’t yet know, and how to plan accordingly.
The Evidence Base for Extended Use
The STEP trial program provides the foundation for understanding semaglutide’s long-term profile.
STEP 1 tracked patients on semaglutide 2.4 mg for 68 weeks. Average weight loss was 14.9% of body weight, maintained throughout the trial period. STEP 5 extended observation to 104 weeks (two full years) and confirmed that weight loss was sustained with no erosion of effectiveness over time. Patients continued to maintain their results at the two-year mark just as well as they had at one year.
STEP 4 provided the most important insight about duration. Patients who achieved stable weight loss on semaglutide were randomized to either continue or switch to placebo. The continuation group maintained their results. The placebo group regained approximately two-thirds of their lost weight within a year. This trial effectively demonstrated that semaglutide’s benefits are dependent on continued use (Rubino et al., JAMA, 2021).
Beyond the STEP program, semaglutide has been available as Ozempic (for type 2 diabetes) since 2017. Real-world data from diabetes patients who’ve used it continuously for five or more years shows no emerging safety signals and sustained metabolic benefits. While the diabetes indication involves different dosing and a different patient population, this real-world track record is reassuring for long-term safety.
The SELECT cardiovascular outcomes trial added another dimension. It showed that semaglutide 2.4 mg reduced major adverse cardiovascular events by 20% in patients with obesity and established cardiovascular disease over a median follow-up of roughly 40 months. This suggests that staying on semaglutide long-term may provide cardiovascular protection above and beyond weight management.
Why Semaglutide Is Meant to Be Taken Continuously
The biology behind this is well understood, even if the implications are still sinking in for many patients.
When you lose weight, your body doesn’t simply accept the new, lower weight as its new normal. It fights back through a coordinated set of hormonal and metabolic adaptations. Ghrelin (your primary hunger hormone) increases. Leptin (which signals fullness) decreases disproportionately relative to your fat loss. Your resting metabolic rate drops, often below what your new weight alone would predict. These adaptations have been documented to persist for years, possibly indefinitely, after weight loss.
Semaglutide works by counteracting this biological resistance. It suppresses appetite through GLP-1 receptor activation in the brain, slows gastric emptying to enhance meal satisfaction, and improves insulin sensitivity. When you take semaglutide away, the counterregulatory hormones are no longer opposed. Hunger returns, satiety diminishes, and weight regain begins.
This isn’t a flaw in the medication. It’s a reflection of how obesity works as a chronic disease. Just as removing blood pressure medication allows blood pressure to rise again, removing semaglutide allows the biological drivers of weight regain to reassert themselves.
The semaglutide timeline covers how weight loss progresses during active treatment. But the more relevant question for long-term planning isn’t how fast you lose. It’s what keeps the weight off. And the answer, based on current evidence, is continued treatment.
What Long-Term Semaglutide Treatment Looks Like
Once you’ve completed dose escalation and reached your maintenance dose, long-term treatment settles into a predictable routine.
The weekly injection becomes automatic. Most long-term patients report that the injection is a non-event. Pick your day, pick your time, inject, move on. The process takes less than a minute, and after several months it requires no more thought than taking a daily vitamin.
Side effects generally decrease over time. The GI side effects that are most common during dose escalation (nausea, constipation, diarrhea) tend to diminish significantly during sustained use. Most patients on a stable dose for six months or longer report minimal or no ongoing side effects. Occasional GI discomfort can still occur, particularly after large or fatty meals, but it’s typically mild and manageable.
Provider visits become less frequent. During the first year, your provider may want to see you every one to three months to monitor progress, adjust dosing, and address side effects. During stable maintenance, visits typically shift to every six months with periodic bloodwork (metabolic panel, thyroid function, lipids, HbA1c if relevant).
Weight stabilizes. After the active weight loss phase (which usually lasts 9 to 18 months depending on your starting point and dose), your weight settles into a new equilibrium. This isn’t a plateau in the frustrating sense. It’s your body reaching a stable point where your intake and expenditure balance at your lower weight with the medication’s support. The goal shifts from losing to maintaining.
Lifestyle habits continue to matter. Semaglutide handles the hormonal aspects of weight maintenance. But resistance training, adequate protein intake, sleep quality, and stress management remain important for overall health, body composition, and metabolic function. The medication and lifestyle work together. Neither is sufficient alone for optimal long-term outcomes.
Safety Considerations for Extended Use
The safety profile of long-term semaglutide use is well-characterized, with a few areas where the picture is still developing.
Well-established and manageable risks. GI side effects are the most common and tend to improve over time. Gallbladder events (gallstones, cholecystitis) occur at slightly elevated rates during rapid weight loss, regardless of method. Monitoring and early intervention manage these effectively.
Rare but serious risks. Pancreatitis has been reported at low rates. Symptoms (severe abdominal pain radiating to the back, nausea, vomiting) warrant immediate medical attention and discontinuation. The risk doesn’t appear to increase with treatment duration.
Theoretical concerns. Medullary thyroid carcinoma was observed in rodent studies at very high doses. It has not been confirmed in human patients. Patients with a personal or family history of MTC or Multiple Endocrine Neoplasia syndrome type 2 (MEN 2) should not take semaglutide. For everyone else, the risk remains theoretical.
Emerging monitoring areas. Bone density is one area getting more attention. Rapid weight loss reduces mechanical loading on bones and can decrease bone mineral density. Long-term GLP-1 use during sustained lower body weight may warrant periodic bone density monitoring, particularly for postmenopausal women. Resistance training and adequate calcium and vitamin D intake help mitigate this concern.
What we don’t yet know. Truly long-term data (10+ years) on semaglutide for weight management doesn’t exist yet because the medication hasn’t been used for that purpose long enough. The existing multi-year data is consistently reassuring, but complete long-term certainty requires more time. Your provider can help you contextualize this uncertainty against the well-documented benefits of continued treatment.
Dose Reduction vs. Full Discontinuation
Many patients and providers are interested in whether a lower maintenance dose can sustain results after the active weight loss phase.
The formal evidence for this approach is limited. Published trials have compared full-dose continuation to complete discontinuation, not to reduced dosing. But the clinical logic is reasonable: if the full dose was needed to drive weight loss, a lower dose might be sufficient to prevent regain, since maintaining a weight is physiologically easier than losing.
In practice, some providers implement a step-down protocol once weight has been stable for three to six months. This might look like reducing from 2.4 mg to 1.7 mg, monitoring for four to eight weeks, and further reducing to 1 mg if weight remains stable. If weight starts trending upward at any point, the dose goes back up.
This approach isn’t guaranteed to work for everyone. Some patients need their full treatment dose to maintain results. Others do well at significantly reduced doses. The only way to know is to try it carefully with close monitoring.
The semaglutide 1-month results article covers what happens at various dose levels during the early phase. Understanding how your body responds at different doses during active treatment can provide some insight into whether dose reduction might work during maintenance, though the dynamics are different.
If cost is the primary reason for exploring dose reduction, compounded semaglutide through TrimRx may be a more straightforward solution. Maintaining your effective dose at a lower monthly cost avoids the uncertainty of whether a reduced dose will hold.
Planning for Interruptions
Even patients committed to long-term use sometimes face treatment interruptions. Insurance changes, medication shortages, financial pressures, or life events (surgery, pregnancy planning, travel) can create gaps.
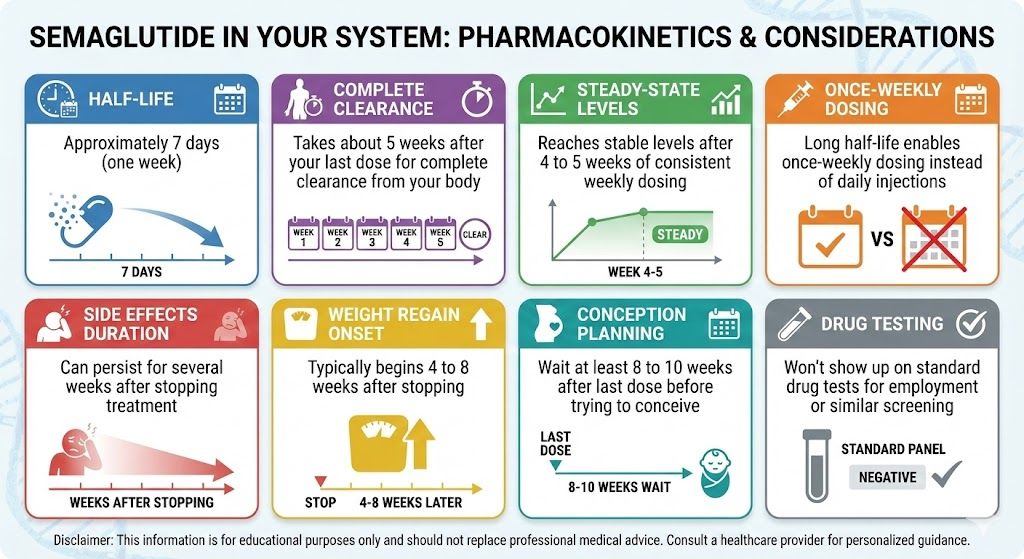
Short gaps (one to two missed doses) generally don’t cause significant issues. Resume at your regular dose on your next scheduled injection day. Appetite may increase slightly during the gap but typically normalizes quickly once you resume.
Longer gaps (three or more weeks) may require a modified restart. Your provider might have you resume at a lower dose and retitrate upward, particularly if you experience GI side effects when restarting. The longer the gap, the more likely your body has partially readjusted to functioning without the medication.
If you anticipate an interruption, plan ahead. Increase dietary vigilance during the gap. Weigh yourself regularly to catch any regain early. Resume treatment as soon as possible. Reaching out to your provider before the interruption allows you to develop a management strategy rather than reacting after the fact.
Switching Medications During Long-Term Treatment
Some patients on long-term semaglutide consider switching to tirzepatide for additional results or renewed progress after a plateau. The tirzepatide weight loss results show that the dual GIP/GLP-1 mechanism produces roughly 5 to 7 percentage points more body weight loss on average than semaglutide alone. For patients who’ve maximized their results on semaglutide but want further improvement, compounded tirzepatide through TrimRx offers an accessible pathway to the dual-receptor approach.
Conversely, some patients on long-term tirzepatide switch to semaglutide for cost or access reasons. Both directions are manageable, and the semaglutide first week article provides context for what the initial semaglutide experience involves, though returning to it after tirzepatide is a different experience than starting fresh.
Building a Sustainable Long-Term Plan
Approaching semaglutide as a long-term treatment means planning for sustainability from the start.
Choose a formulation and provider you can maintain. If brand pricing isn’t sustainable over years, start with compounded semaglutide rather than switching later. TrimRx offers a telehealth model designed for ongoing GLP-1 treatment with consistent pricing and regular provider access.
Establish monitoring routines. Bloodwork every six to twelve months, regular weigh-ins, and periodic check-ins with your provider keep you on track and catch any emerging issues early.
Invest in the lifestyle foundation. Resistance training, protein-focused nutrition, quality sleep, and stress management aren’t optional extras. They’re the base that makes long-term medication use most effective and supports your overall health beyond what any medication can do alone.
Have the cost conversation early. Know what you’ll pay monthly, how your insurance works, and what alternatives exist if coverage changes. The patients who maintain treatment longest are usually the ones who’ve planned for the financial aspect from the beginning.
If you’re ready to build a long-term treatment plan, TrimRx’s intake quiz connects you with a provider who can help you choose the right medication, dose, and approach for sustainable, ongoing weight management.
This information is for educational purposes and is not medical advice. Consult with a healthcare provider before starting any medication. Individual results may vary.

Transforming Lives, One Step at a Time
Keep reading
Semaglutide to Tirzepatide: Switching Guide
Switching from semaglutide to tirzepatide is one of the most clinically supported medication transitions in GLP-1 weight loss treatment. You’re moving from a single-receptor…
Semaglutide Stopped Working: Next Steps
If semaglutide was producing steady weight loss and then stopped, you’re experiencing a plateau, and it’s one of the most common phases in GLP-1…
Semaglutide First Week: What Happens to Your Body
Your first week on semaglutide probably won’t bring dramatic weight loss, and that’s completely by design. The starting dose of 0.25 mg is intentionally…



