How Much Does Ozempic Cost? 2026 Pricing Guide and Affordable Alternatives

You’re considering Ozempic for weight loss, but when you look up the price, the numbers stop you cold. The sticker shock is real, and you’re wondering if effective weight loss medication is simply out of reach.
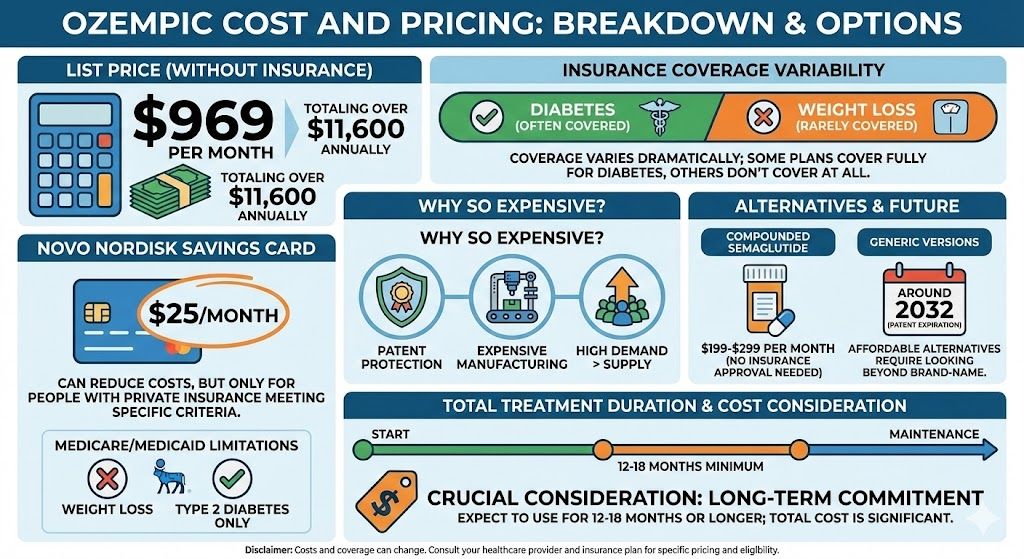
Here’s the straightforward answer: Ozempic costs approximately $969 per month without insurance. That’s over $11,600 annually for a medication you’ll likely need for 12-18 months or longer to achieve and maintain significant weight loss. But the actual cost you’ll pay depends on several factors, including your insurance coverage, whether you qualify for manufacturer savings programs, and whether you’re open to clinically equivalent alternatives that cost 80% less.
This guide breaks down Ozempic’s actual costs, explains why it’s so expensive, covers insurance and savings options, and presents affordable alternatives that use the same active ingredient at a fraction of the price.
Key Takeaways: Ozempic Cost and Pricing
- Ozempic’s list price is $969 per month without insurance coverage, totaling over $11,600 annually.
- Insurance coverage varies dramatically—some plans cover it fully for diabetes but not weight loss, while others don’t cover it at all.
- Novo Nordisk’s savings card can reduce costs to as little as $25/month, but only for people with private insurance who meet specific eligibility criteria.
- Medicare and Medicaid typically do not cover Ozempic for weight loss, only for type 2 diabetes treatment.
- The high cost stems from patent protection, expensive manufacturing processes, and significant demand that outpaces supply.
- Compounded semaglutide offers the same active ingredient at $199-$299 per month without requiring insurance approval.
- Treatment duration matters significantly—expect to use Ozempic for 12-18 months minimum, potentially longer for maintenance, making total cost a crucial consideration.
- Generic versions won’t be available until patents expire around 2032, meaning affordable alternatives require looking beyond brand-name options.
Understanding Ozempic’s List Price
Ozempic’s manufacturer, Novo Nordisk, sets the wholesale acquisition cost at approximately $969 per month. This price covers one pen containing four weekly doses (enough for a month of treatment). Pharmacies typically add a markup to this base price, so your actual retail cost might range from $950 to $1,000 depending on where you fill the prescription.
This pricing applies whether you’re taking the 0.25mg/0.5mg starter dose or the maintenance doses of 1mg or 2mg. Unlike some medications where higher doses cost more, Ozempic pens are priced per pen regardless of the dosage strength.
To put this in perspective, a year of Ozempic treatment at list price costs more than $11,600. For many people seeking weight loss medication, this represents 15-20% or more of their annual income. The financial barrier is substantial and prevents many people from accessing what could be genuinely life-changing treatment.
The cost becomes even more significant when you consider that Ozempic isn’t a short-term solution. Clinical trials showing the medication’s effectiveness typically ran for 68 weeks or longer. Most people need at least 12-18 months of treatment to achieve their weight loss goals, and many require ongoing maintenance doses to prevent weight regain.
Why Does Ozempic Cost So Much?
Several factors contribute to Ozempic’s high price tag, and understanding them helps explain why affordable alternatives have become so important.
Patent Protection and Market Exclusivity
Novo Nordisk holds patents on semaglutide that extend through 2032. During this exclusivity period, no generic competitors can enter the market, allowing the manufacturer to set prices without competitive pressure. This patent protection is standard in pharmaceutical development, designed to help companies recoup the substantial research and development costs for new drugs.
Manufacturing Complexity
Semaglutide is a GLP-1 receptor agonist that requires sophisticated biotechnology manufacturing processes. Unlike simple chemical compounds that can be synthesized relatively easily, GLP-1 medications involve complex molecular structures that are expensive to produce. The manufacturing requires specialized facilities, extensive quality control, and sophisticated cold-chain logistics for distribution.
Research and Development Costs
Novo Nordisk invested billions in developing semaglutide, conducting extensive clinical trials that followed thousands of participants over multiple years. The STEP clinical trial program alone involved over 4,500 participants across multiple studies. These trials are enormously expensive, and pharmaceutical companies typically price medications to recoup these investments.
Demand Outpacing Supply
The explosive popularity of GLP-1 medications for weight loss has created supply constraints. When demand far exceeds supply, manufacturers have little incentive to lower prices. Novo Nordisk has struggled to keep up with demand, leading to periodic shortages that further complicate access for patients.
Marketing and Distribution Costs
Novo Nordisk spends substantial amounts on marketing to healthcare providers and consumers. While controversial, these costs factor into the medication’s pricing structure. The company also maintains patient support programs, training materials for healthcare providers, and extensive distribution networks.
Insurance Coverage: The Complicated Reality
Insurance coverage for Ozempic varies dramatically depending on your specific plan, whether you have a diagnosis of type 2 diabetes, and whether your insurer covers weight loss medications at all.
Type 2 Diabetes Coverage
Most insurance plans cover Ozempic when prescribed for type 2 diabetes management, its FDA-approved indication. However, coverage doesn’t mean free. You’ll typically face:
- Copays ranging from $25-$100 per month with commercial insurance
- Prior authorization requirements showing you’ve tried other diabetes medications first
- Step therapy protocols requiring failure on metformin or other first-line treatments
- Quantity limits restricting how much you can fill at once
Even with insurance coverage for diabetes, many plans implement these barriers that can delay access to the medication for weeks or months.
Weight Loss Coverage: Mostly Excluded
Here’s where insurance becomes problematic for most people interested in Ozempic for weight loss. The majority of insurance plans specifically exclude coverage for weight loss medications, even when prescribed by a physician for obesity management.
Many insurers distinguish between Ozempic (approved for diabetes) and Wegovy (the same medication approved specifically for weight loss at a 2.4mg dose). If you’re prescribed Ozempic off-label for weight loss without a diabetes diagnosis, most insurance plans will deny the claim outright. This is true even though the medications contain identical active ingredients and Ozempic is widely prescribed for weight loss.
Medicare and Medicaid Limitations
Medicare Part D plans generally cannot cover medications prescribed for weight loss due to federal law. Medicare may cover Ozempic only if you have a type 2 diabetes diagnosis, and even then, costs can be substantial depending on your specific plan and whether you’re in the coverage gap (the “donut hole”).
Medicaid coverage varies by state. Some states cover GLP-1 medications for diabetes but not weight loss, while others have implemented strict utilization management programs requiring extensive documentation before approval.
Commercial Insurance Variability
If you have private insurance through an employer, coverage depends entirely on what your employer’s plan includes. Some employers specifically exclude weight loss medications to control premium costs. Others may cover Wegovy but not Ozempic for weight loss, or vice versa, depending on their pharmacy benefit negotiations.
The unpredictability of insurance coverage means you can’t assume you’ll have access to Ozempic at an affordable price simply because you have health insurance. Many people with excellent insurance coverage for other medical needs find themselves paying full retail price for weight loss medications.
Manufacturer Savings Programs and Coupons
Novo Nordisk offers savings programs that can substantially reduce Ozempic’s cost, but these programs have significant limitations and eligibility requirements.
The Ozempic Savings Card
Novo Nordisk’s most prominent savings offer is a card that can reduce monthly costs to as little as $25 for commercially insured patients. This sounds like an excellent deal, but the restrictions are substantial:
You must have commercial (private) health insurance. The card doesn’t work if you’re uninsured, or if you have government insurance like Medicare, Medicaid, or TRICARE. This immediately excludes millions of Americans from the program.
Your insurance must provide some coverage for Ozempic. The savings card covers out-of-pocket costs up to a maximum benefit limit, but your insurance must process the claim first. If your insurance denies the claim entirely (common for weight loss prescriptions), the savings card won’t help.
There’s a maximum annual benefit, typically around $150 per fill with certain yearly caps. Once you reach these limits, you’re responsible for the remaining costs. For some people on high-deductible plans, this benefit gets exhausted quickly.
You must meet certain BMI requirements and have your prescription written for an FDA-approved indication. Getting a prescription written “off-label” for weight loss may disqualify you from using the savings card.
Patient Assistance Programs
Novo Nordisk also operates a patient assistance program for uninsured or underinsured patients who meet income requirements. This program can provide medication at no cost, but qualification is stringent:
Your household income must fall below certain thresholds (typically 400% of the federal poverty level or less, depending on household size). You must be a U.S. citizen or legal resident. You cannot have insurance coverage that would pay for Ozempic. You must reapply annually and provide extensive financial documentation.
For many people struggling with Ozempic’s cost, they earn too much to qualify for assistance programs but not enough to comfortably afford $900+ monthly out of pocket.
Pharmacy Discount Cards
Various pharmacy discount card programs promise savings on prescription medications. However, these typically provide modest discounts on Ozempic—perhaps reducing the price from $969 to $850 or $900. While any savings help, these discounts still leave the medication financially out of reach for most people.
The fundamental issue with all manufacturer savings programs is that they’re designed primarily for people who already have insurance coverage. If you’re uninsured or your insurance explicitly excludes weight loss medications, these programs offer limited help.
Affordable Alternatives: Compounded Semaglutide
The emergence of compounded semaglutide has transformed access to GLP-1 weight loss medications, offering the same active ingredient at 75-80% lower costs than brand-name Ozempic.
What Is Compounded Semaglutide?
Compounded medications are prepared by licensed pharmacies that combine active pharmaceutical ingredients into customized formulations. During periods when FDA-approved medications are in shortage (as semaglutide has been intermittently), compounding pharmacies can legally prepare medications using the same active ingredient.
Compounded semaglutide contains the identical active ingredient as Ozempic—semaglutide—but is typically provided in vials for injection rather than the pre-filled pen devices that brand-name products use. The medication works the same way in your body and follows the same dosing schedules from 0.25mg to 2mg weekly.
Cost Comparison
Compounded semaglutide through TrimRx costs $199 per month, representing an 80% savings compared to Ozempic’s $969 monthly price. This lower cost holds consistent regardless of your insurance status, making it accessible to people whose insurance doesn’t cover weight loss medications.
Over a typical 18-month treatment course, the cost difference is substantial:
- Ozempic: $17,442 (at list price without insurance)
- Compounded semaglutide: $3,582 (at $199/month)
- Total savings: $13,860
Even if you have insurance that covers some portion of Ozempic costs, compounded alternatives often cost less than high copays or coinsurance amounts on commercial plans.
Safety and Effectiveness
Compounded semaglutide uses the same active pharmaceutical ingredient as brand-name Ozempic. The chemical compound (semaglutide) is identical—what differs is the delivery method and the absence of the convenient pre-filled pen. Clinical outcomes depend on the active ingredient reaching your system at appropriate doses, which properly compounded medications achieve.
Reputable telehealth platforms like TrimRx work with FDA-registered compounding pharmacies that follow strict quality standards. These pharmacies must meet the same pharmaceutical manufacturing requirements as facilities producing brand-name medications. Compounded medications undergo testing for potency, sterility, and stability to ensure they meet safety standards.
The Trade-Offs
Compounded medications require you to measure and inject doses yourself using vials and syringes, rather than the simple click-mechanism of Ozempic pens. Many people find this adjustment straightforward after initial training, but it does require slightly more preparation time.
Compounded medications may not be suitable if you have difficulty with manual dexterity or vision problems that make measuring precise doses challenging. However, for most people, the significant cost savings far outweigh this minor inconvenience.
The legal status of compounded GLP-1 medications depends on shortage designations. If the FDA removes semaglutide from the shortage list, compounding pharmacies’ ability to prepare these medications may change. However, given persistent supply constraints, semaglutide has remained on shortage lists for extended periods.
Comparing Total Treatment Costs
Understanding the true cost of Ozempic requires looking beyond monthly prices to the total investment over a complete treatment course. Most people use GLP-1 medications for 12-24 months to achieve and stabilize their weight loss, making long-term costs crucial to consider.
12-Month Treatment Comparison
Without insurance or assistance programs:
- Ozempic: $11,628 ($969 × 12 months)
- Compounded semaglutide: $2,388 ($199 × 12 months)
- Savings with compounded: $9,240
With insurance and Ozempic savings card (best-case scenario of $25/month copay):
- Ozempic: $300 ($25 × 12 months)
- Compounded semaglutide: $2,388 ($199 × 12 months)
In the best-case scenario with excellent insurance coverage and qualification for maximum savings card benefits, brand-name Ozempic is cheaper. However, this scenario applies to a minority of patients. Most people face monthly costs somewhere between $25 and $969, depending on their specific insurance situation.
18-Month Treatment Comparison
For an 18-month treatment course (common for achieving significant weight loss):
- Ozempic without assistance: $17,442
- Compounded semaglutide: $3,582
- Difference: $13,860
This substantial difference explains why many people choose compounded alternatives even when they could potentially access brand-name options through insurance with prior authorization battles and uncertainty about ongoing coverage.
Maintenance Phase Costs
Many people require lower maintenance doses after achieving their target weight to prevent regain. Whether you continue with the same dose or reduce to a lower maintenance dose, the cost structure remains similar. The ongoing financial commitment is an important consideration when starting treatment. Clinical evidence from studies like STEP 4 showed that discontinuing semaglutide led to significant weight regain in most participants, suggesting that long-term or indefinite use may be necessary for sustained results.
Does Location Affect Ozempic Cost?
Pharmacy pricing varies modestly by location and pharmacy chain, but the differences are relatively small compared to Ozempic’s overall high cost.
Pharmacy Chain Comparisons
Major pharmacy chains (CVS, Walgreens, Walmart, Costco, etc.) typically price Ozempic within $50-100 of each other at list price. Costco often offers slightly lower prices, sometimes $875-925 per month compared to $950-1,000 at other chains, but you need a Costco membership to access their pharmacy.
Specialty pharmacies that insurance companies designate for certain medications may offer different pricing, and some plans require you to use specific pharmacies to receive coverage. This adds another layer of complexity to predicting your actual costs.
State-Level Pricing Differences
Unlike some medications where prices vary substantially by state, Ozempic maintains relatively consistent list pricing across the United States. The manufacturer sets wholesale pricing uniformly, and while individual pharmacies might add different markups, these variations are modest.
International Pricing
Ozempic costs significantly less in other countries where government healthcare systems negotiate medication prices. Patients in Canada, the UK, and many European countries pay far less for the same medication. However, importing medications from other countries to save money involves legal complications and risks regarding medication authenticity and storage conditions during transit. Most healthcare providers advise against purchasing medications from international sources due to these concerns.
When Generic Ozempic Might Become Available
If you’re hoping that generic semaglutide will eventually solve the cost problem, you’ll be waiting a long time.
Novo Nordisk’s patents on semaglutide extend through 2032. Until these patents expire, generic manufacturers cannot legally produce identical versions of Ozempic in the United States. This means at least seven more years (as of 2026) before generic competition could potentially lower prices through market forces.
Even when patents expire, generic availability isn’t guaranteed immediately. Manufacturers must conduct studies proving their generic versions are bioequivalent to the brand-name product, then submit these for FDA approval. This process takes additional time after patent expiration.
The complex biotechnology manufacturing required for GLP-1 medications like semaglutide also means that generic production may be more challenging and expensive than generic versions of simpler chemical compounds. Generic biologics (called “biosimilars”) typically offer smaller discounts compared to the brand-name versions than traditional generic medications do.
Given this timeline, waiting for generic semaglutide isn’t a practical strategy for people who would benefit from treatment now. The years lost waiting for generic availability represent years when the medication could be helping with weight management, metabolic health improvements, and reducing obesity-related health risks.
Making the Cost Decision: What Makes Sense for You
Deciding whether Ozempic’s cost is manageable requires honest assessment of your financial situation, treatment needs, and available alternatives.
If You Have Insurance
Contact your insurance provider before filling a prescription. Ask specifically:
- Does your plan cover Ozempic, and for what indications (diabetes, weight loss, or both)?
- What will your copay or coinsurance cost be after meeting any deductible?
- Is prior authorization required, and what’s the approval process timeline?
- Are there step therapy requirements that need to be completed first?
- Would the Novo Nordisk savings card work with your insurance plan?
Many people find that their insurance will cover Ozempic for diabetes but not weight loss, leaving them to pay full price despite having health insurance. Understanding your specific coverage before starting treatment prevents unpleasant financial surprises.
If You’re Uninsured or Underinsured
For people without insurance coverage for weight loss medications, compounded alternatives provide access to the same treatment at costs that are manageable within many household budgets. At $199 monthly, compounded semaglutide costs less than many family cell phone plans, gym memberships, or other routine monthly expenses.
Consider the broader financial picture. Obesity contributes to numerous health conditions that themselves carry substantial costs—type 2 diabetes management, blood pressure medications, joint problems requiring treatment, and increased risk of serious conditions like heart disease and certain cancers. Investing in effective weight loss treatment now may reduce future healthcare costs significantly.
Budgeting for Treatment Duration
Don’t just consider monthly costs—think about the total investment over the time you’ll need treatment. If paying $969 monthly for Ozempic would strain your finances to the point of potentially having to discontinue treatment prematurely, starting with a more affordable alternative that you can sustain long-term makes more sense.
Clinical trials showing semaglutide’s effectiveness typically followed participants for 68 weeks (about 16 months). Real-world use often extends longer. Budgeting for at least 12-18 months of treatment provides a realistic financial picture.
Considering Alternative Medications
Tirzepatide (brand names Mounjaro and Zepbound) represents another GLP-1 medication option, though it comes with similar cost challenges. Zepbound lists at $1,069 monthly—even more expensive than Ozempic. However, tirzepatide showed superior weight loss results in head-to-head comparisons, with participants losing an average of 22.5% of body weight compared to 14.9% with semaglutide in the SURMOUNT-2 trial.
Compounded tirzepatide at $349 monthly through TrimRx offers another affordable alternative with potentially better results. Your choice between semaglutide and tirzepatide should consider both effectiveness and cost. Our complete Ozempic vs Mounjaro comparison can help you understand the differences between these medications.
Frequently Asked Questions
How much does Ozempic cost at different pharmacies?
Ozempic costs approximately $950-$1,000 per month at most major U.S. pharmacies without insurance. CVS, Walgreens, Walmart, and other chains price the medication within $50 of each other. Costco sometimes offers slightly lower pricing around $875-925, but requires a membership. Mail-order pharmacies through your insurance plan may offer different pricing, potentially lower if your plan incentivizes using specific pharmacies.
Can I get Ozempic for free or at very low cost?
Free or very low-cost Ozempic is possible but rare and requires specific circumstances. The Novo Nordisk patient assistance program provides free medication to uninsured patients who meet income requirements (typically below 400% of federal poverty level). The manufacturer’s savings card can reduce costs to $25/month for commercially insured patients whose plans cover Ozempic, but this excludes Medicare, Medicaid, and uninsured patients. Most people don’t qualify for these programs or find compounded alternatives at $199/month more accessible than navigating assistance program requirements.
Why doesn’t insurance cover Ozempic for weight loss?
Most insurance plans specifically exclude coverage for weight loss medications as a cost-control measure, even when prescribed by physicians for obesity management. This exclusion exists because insurers view weight loss medications as “lifestyle” drugs rather than treatments for medical conditions, despite obesity being recognized as a chronic disease. Many plans will cover Ozempic for type 2 diabetes (its FDA-approved indication) but deny claims when prescribed for weight loss without a diabetes diagnosis. Some employers specifically negotiate to exclude weight loss medication coverage from their health plans to keep premiums lower.
How long will I need to take Ozempic?
Most people use Ozempic for at least 12-18 months to achieve significant weight loss, based on the duration of clinical trials that demonstrated the medication’s effectiveness. Many individuals require ongoing maintenance treatment to prevent weight regain after reaching their target weight. The STEP 4 trial showed that participants who discontinued semaglutide regained approximately two-thirds of their lost weight within one year. This suggests that long-term or potentially indefinite use may be necessary for sustained results, making total treatment cost over multiple years an important consideration when deciding whether Ozempic or alternatives are financially sustainable.
Is compounded semaglutide really the same as Ozempic?
Compounded semaglutide contains the same active pharmaceutical ingredient as brand-name Ozempic—the chemical compound is identical. The difference lies in the delivery method: Ozempic comes in pre-filled pens while compounded versions typically come in vials requiring self-measurement and injection. When prepared by licensed, FDA-registered compounding pharmacies following proper pharmaceutical standards, compounded semaglutide is clinically equivalent and follows the same dosing protocols. The medication works identically in your body at equivalent doses. Quality compounding pharmacies test their preparations for potency, sterility, and stability to ensure they meet safety and effectiveness standards.
What happens if I can’t afford to continue Ozempic?
Discontinuing Ozempic typically leads to weight regain in most people, according to clinical trials. The STEP 4 study found that participants who stopped semaglutide regained about two-thirds of their lost weight within a year. If brand-name Ozempic becomes financially unsustainable, transitioning to compounded semaglutide at $199 monthly allows you to continue treatment at lower cost rather than discontinuing entirely. Planning for the full treatment duration cost before starting helps prevent the difficult situation of needing to stop treatment mid-course for financial reasons. Our guide on stopping Ozempic and managing weight regain provides strategies if discontinuation becomes necessary.
Does FSA or HSA money work for Ozempic?
Flexible Spending Accounts (FSA) and Health Savings Accounts (HSA) can typically be used to pay for Ozempic if you have a prescription from your healthcare provider. However, your FSA/HSA administrator might require documentation that the medication is prescribed for a medical condition (such as type 2 diabetes) rather than for weight loss specifically, depending on their policies. Some plans restrict using tax-advantaged healthcare accounts for weight loss medications. Check with your specific FSA or HSA administrator about their requirements. Using FSA/HSA funds doesn’t reduce Ozempic’s overall cost but does provide tax advantages by using pre-tax dollars.
How much does Ozempic cost with Medicare?
Medicare Part D prescription drug plans can cover Ozempic only if prescribed for type 2 diabetes management, not for weight loss. Federal law prohibits Medicare from covering weight loss medications. For diabetes treatment, your cost depends on your specific Part D plan, what tier Ozempic falls into on your plan’s formulary, and whether you’re in the deductible phase or coverage gap (donut hole). Most Medicare beneficiaries face substantial out-of-pocket costs ranging from $200-$600 monthly even with Part D coverage. The Novo Nordisk savings card doesn’t work with Medicare, leaving many seniors unable to afford brand-name Ozempic even with insurance.
Can I split Ozempic pens to make them last longer?
Ozempic pens are designed for exactly four weekly doses at the prescribed strength. Each pen click dispenses one week’s dose, and the pen contains enough medication for one month of treatment. You cannot adjust the pen to dispense smaller amounts to make it last longer—the click mechanism is fixed. Attempting to modify how you use the pen could result in inaccurate dosing, which affects both effectiveness and safety. Proper semaglutide dosing follows a specific titration schedule starting at 0.25mg and gradually increasing. Taking less than prescribed doses means you won’t achieve the full benefits the medication offers.
Are there patient advocacy programs that help with Ozempic costs?
Several nonprofit organizations work to help patients access medications they can’t afford, including the Patient Advocate Foundation, NeedyMeds, and RxAssist. These organizations provide information about assistance programs and sometimes direct financial help for medication costs. However, most advocacy programs focus on medications for serious acute conditions rather than chronic weight management medications. The most reliable assistance for Ozempic comes directly from Novo Nordisk’s patient assistance program for qualifying uninsured patients, though income requirements exclude many people who still struggle with the medication’s cost. Exploring compounded alternatives often provides more reliable access than navigating uncertain assistance programs.
Finding Affordable Access to Semaglutide Treatment
The cost of Ozempic represents a significant barrier for many people who would benefit from GLP-1 medication for weight loss. At $969 monthly without insurance, and with many insurance plans excluding weight loss medication coverage entirely, brand-name options remain financially out of reach for a large portion of the population that could achieve meaningful health improvements through treatment.
Understanding your actual costs requires investigating your specific insurance coverage, determining whether you qualify for manufacturer assistance programs, and realistically assessing whether you can sustain the expense over 12-18 months or longer. For most people without excellent insurance coverage that includes weight loss medications, the math simply doesn’t work for brand-name Ozempic at full retail price.
The emergence of compounded semaglutide has fundamentally changed this calculation. The same active ingredient that makes Ozempic effective—semaglutide—is available through licensed compounding pharmacies at 75-80% lower costs. This isn’t a compromise on the medication itself; it’s the same chemical compound prepared by qualified pharmacies following pharmaceutical standards, just delivered in vials rather than disposable pens.
Whether you’re using brand-name Ozempic with strong insurance coverage or affordable compounded semaglutide at $199 monthly through TrimRx, the medication’s effectiveness depends on consistent use over an extended period, following proper dosing protocols, and incorporating it into comprehensive lifestyle changes. The best medication is the one you can actually afford to take consistently for as long as you need it. Get started with comprehensive medical support, affordable pricing, and convenient online access to semaglutide treatment that works within your budget.

Transforming Lives, One Step at a Time
Keep reading
Online Ozempic Prescription Texas
You can get an Ozempic prescription online in Texas through a licensed telehealth provider without an in-person visit. Texas telehealth law allows providers to…
Online Ozempic Prescription California
You can get an Ozempic prescription online in California through a licensed telehealth provider without an in-person visit. California’s telehealth laws allow providers to…
Weight Loss Clinic Online Texas: Your Options
An online weight loss clinic in Texas gives you access to GLP-1 medications like semaglutide and tirzepatide through a fully virtual process. You complete…



