Life After Ozempic: Maintaining Weight Loss Long-Term

Whether you’re considering stopping Ozempic, have already stopped, or are planning ahead for the possibility, understanding what happens after treatment ends is essential for making informed decisions. The question of life after Ozempic is one of the most important and most misunderstood aspects of GLP-1 treatment.
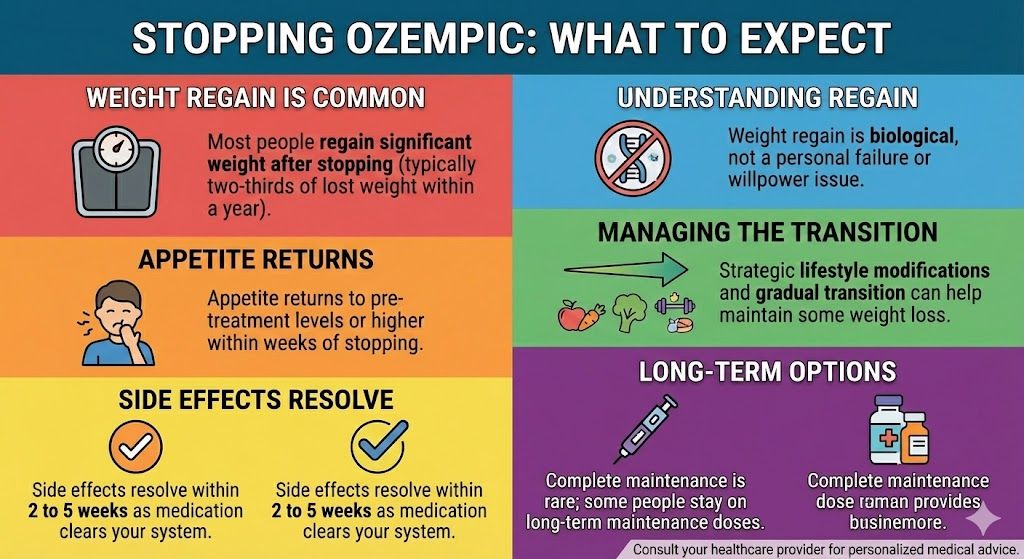
The honest reality: Most patients who stop Ozempic regain a significant portion of their lost weight. Research shows approximately two-thirds of lost weight typically returns within one year of stopping. This isn’t a failure of willpower or a flaw in the medication—it reflects the biological nature of obesity as a chronic condition that the medication was managing, not curing.
This doesn’t mean stopping is never appropriate or that no one maintains their weight loss. Some patients do successfully transition off medication, particularly those who’ve lost more modest amounts, made substantial lifestyle changes, and whose eating wasn’t primarily driven by biological factors that semaglutide addresses. Understanding the patterns, challenges, and strategies gives you the best chance of success if you do stop, and helps you make an informed choice about whether stopping is right for you.
This guide covers:
- What the research shows about weight regain after stopping
- Why weight returns (the biology behind regain)
- Who is most likely to maintain weight loss without medication
- Strategies for those who stop taking Ozempic
- How to transition off the medication
- Building a sustainable post-medication lifestyle
- Warning signs that you may need to restart
- Making an informed decision about stopping
- The case for continued treatment
- Realistic expectations for life after Ozempic
Key Takeaways
- Weight regain after stopping is the norm, not the exception—approximately two-thirds of lost weight typically returns within one year
- Biological factors drive regain: Appetite regulation, metabolic adaptation, and hormonal signals push toward previous weight
- The medication manages, doesn’t cure: Stopping removes the management tool while the underlying condition remains
- Some patients do maintain successfully, particularly those with modest weight loss goals and substantial lifestyle changes
- Gradual lifestyle solidification during treatment improves chances of maintaining some loss after stopping
- Early intervention if weight regains can prevent returning to baseline weight
- Restarting isn’t failure: Many patients stop, regain, and successfully restart treatment
- The decision to stop is personal and should weigh benefits, costs, and realistic expectations
- Continued treatment remains an option and is the most reliable way to maintain results
- Whatever you decide, understanding the likely outcomes helps you make an informed choice
What Research Shows About Stopping
Understanding the data helps set realistic expectations.
The STEP 1 Extension Study
The most direct evidence about what happens after stopping semaglutide comes from an extension of the landmark STEP 1 trial:
Study design:
- Patients took semaglutide 2.4mg for 68 weeks
- Average weight loss: 14.9% of body weight
- Medication was then stopped
- Patients were followed for one additional year off medication
Results after one year without medication:
- Patients regained approximately two-thirds of lost weight
- From 14.9% loss, weight returned to approximately 5-6% below starting weight
- Weight was still trending upward at end of follow-up
What this means practically:
- Initial weight: 220 pounds
- After 68 weeks on semaglutide: 187 pounds (33 pounds lost)
- One year after stopping: ~209 pounds (22 pounds regained)
- Net maintained loss: ~11 pounds (about one-third of original loss)
Other Supporting Evidence
SUSTAIN studies (diabetes indication):
- Similar patterns of glucose worsening after stopping
- HbA1c returned toward baseline after discontinuation
- Benefits required continued treatment
Real-world observations:
- Clinical experience confirms trial findings
- Weight regain is consistently observed
- Timing and degree vary, but the pattern is reliable
The Trajectory of Regain
How regain typically unfolds:
First 1-3 months:
- Weight may initially remain stable
- Appetite begins returning
- Eating patterns start shifting
- Some patients notice no immediate change
Months 3-6:
- Weight typically begins increasing
- Appetite noticeably higher than during treatment
- Former eating behaviors re-emerge
- Regain becomes apparent
Months 6-12:
- Regain continues progressively
- May slow as approaching previous weight
- Appetite and eating patterns often similar to pre-treatment
- Two-thirds of lost weight typically regained by this point
Beyond one year:
- Trend may continue toward original weight
- Some patients stabilize at partial regain
- Others return fully to baseline
- Limited long-term data beyond one year
Why Weight Returns After Stopping
Understanding the biological mechanisms explains why willpower alone typically can’t prevent regain.
Appetite Regulation Returns to Baseline
What semaglutide was doing:
- Suppressing appetite through GLP-1 receptors in the brain
- Reducing hunger signals
- Enhancing satiety after meals
- Decreasing food preoccupation and cravings
What happens when you stop:
- GLP-1 receptor activation ends
- Appetite returns to pre-treatment levels
- Hunger signals intensify
- The “food noise” returns
- Eating the amount you ate on medication now feels restrictive
The subjective experience:
- Feeling hungrier than you have in months
- Less satisfied after meals
- Thinking about food more often
- Cravings re-emerging
- Fighting constant urges to eat more
Metabolic Adaptation Works Against You
The challenge of lower weight:
- At lower body weight, you need fewer calories to maintain
- A person at 187 pounds burns fewer calories than at 220 pounds
- But appetite doesn’t automatically adjust to match lower caloric needs
Example:
- At 220 pounds, you might burn ~2,400 calories daily
- At 187 pounds, you might burn ~2,100 calories daily
- That’s 300 fewer calories per day to maintain
- Without medication, appetite pushes toward the higher amount
Metabolic adaptation compounds this:
- Weight loss causes additional metabolic slowdown
- Your body becomes more efficient at using calories
- Hormones shift to promote weight regain
- This “starvation response” persists even at healthy weights
Hormonal Signals Favor Regain
Ghrelin (hunger hormone):
- Increases after weight loss
- Signals increased hunger
- Pushes toward eating more
Leptin (satiety hormone):
- Decreases with weight loss
- Less signal that you’re satisfied
- Takes long time (possibly years) to reset
Other hormones:
- Insulin, PYY, GLP-1 (natural), and others affected
- Overall hormonal environment favors weight regain
- These changes can persist for years after weight loss
The Body Defends Previous Weight
Set point theory:
- The body has regulatory mechanisms that “defend” a certain weight
- Weight loss is perceived as a threat
- Multiple systems coordinate to restore previous weight
- This is an evolved survival mechanism, not a character flaw
What this means:
- Regain isn’t about lacking willpower
- Your biology is actively working against maintenance
- The medication was overriding these systems
- Without it, they reassert themselves
Gastric Emptying Normalizes
During treatment:
- Semaglutide slowed stomach emptying
- Food stayed in stomach longer
- This contributed to prolonged fullness
After stopping:
- Gastric emptying returns to normal speed
- Fullness after meals is shorter
- You feel ready to eat again sooner
- May contribute to eating more frequently
Who Successfully Maintains Without Medication?
While most patients regain weight, some do maintain. Understanding the factors associated with success helps set realistic expectations.
Factors Associated With Better Maintenance
Modest weight loss goals:
- Patients who lost smaller amounts (10-15% vs. 20%+) may maintain more easily
- Less dramatic metabolic adaptation
- Smaller gap between previous and current weight
Substantial lifestyle changes:
- Those who genuinely transformed eating habits
- Regular physical activity established as routine
- New relationship with food developed during treatment
- Skills and habits that provide some independent support
Lower initial weight:
- Patients starting with less to lose may maintain more easily
- Less biological pressure toward higher weight
Physical activity:
- Regular exercisers may maintain better
- Activity independently affects appetite and metabolism
- Resistance training preserves muscle mass
Psychological factors:
- Those whose eating wasn’t primarily biologically driven
- Patients who addressed emotional eating patterns
- Those with strong intrinsic motivation and support systems
Time on treatment:
- Longer treatment duration may allow more habit consolidation
- More time for lifestyle changes to become automatic
- Though biological factors remain regardless of duration
Realistic Assessment
Honest questions to ask yourself:
About your eating:
- Was my overeating primarily driven by biological hunger, or by emotional/behavioral factors?
- Have I genuinely changed my eating patterns, or was I relying on reduced appetite?
- Can I maintain my current eating if appetite returns to previous levels?
About your lifestyle:
- Have I established sustainable exercise habits?
- Are my new eating patterns automatic, or do they require constant effort?
- What was my relationship with food before treatment?
About your history:
- Have I successfully maintained weight loss before?
- What happened when I stopped previous diets or weight loss programs?
- What’s different now?
About your expectations:
- Am I prepared for my appetite to return?
- Do I have a plan if weight starts increasing?
- Am I willing to restart medication if needed?
The Minority Who Maintain
Some patients do maintain significant weight loss after stopping:
What they typically share:
- Achieved more modest weight loss (10-15%)
- Exercise became a genuine lifestyle component
- Made sustainable dietary changes (not extreme restriction)
- Had strong support systems
- Were vigilant about early regain and took action quickly
- Some combination of factors that created sustainable equilibrium
Important context:
- These are the minority, not the majority
- Even among “successful” maintainers, some regain still occurs
- Success often means maintaining most of the loss, not all of it
- Many who initially maintained eventually regained over longer periods
Strategies for Those Who Stop
If you’ve decided to stop Ozempic or have already stopped, these strategies give you the best chance of maintaining your results.
Before Stopping: Preparation Phase
Solidify habits while still on medication:
- The reduced appetite from medication is a window of opportunity
- Use this time to build sustainable eating patterns
- Establish exercise routines that will continue
- Develop skills for managing hunger and cravings
Build your support infrastructure:
- Identify accountability partners
- Consider working with a dietitian or coach
- Establish monitoring systems (regular weigh-ins)
- Plan how you’ll handle challenges
Set realistic expectations:
- Understand that some regain is likely
- Define what you consider acceptable (e.g., maintaining most of your loss)
- Plan what you’ll do if weight exceeds certain thresholds
- Decide in advance when you’d consider restarting medication
How to Transition Off
Gradual vs. abrupt discontinuation:
Abrupt stopping:
- Simply stop taking the medication
- No medical need for tapering
- May experience faster return of appetite
Gradual reduction:
- Step down through lower doses before stopping
- May provide psychological preparation
- Allows you to experience increasing appetite gradually
- No proven benefit for maintenance, but some prefer this approach
Either approach is medically acceptable. Choose based on your preference and provider’s recommendation.
The First Weeks and Months
What to expect:
- Appetite will return, possibly intensely
- May feel like you’re constantly hungry initially
- Portion sizes that felt satisfying may feel inadequate
- Food may become more mentally prominent
Strategies:
- Expect the appetite return; don’t be caught off guard
- Have structured eating plans in place
- Use protein and fiber to maximize satiety
- Keep problematic foods out of easy access
- Plan meals in advance
- Practice delay tactics for cravings
Nutrition Strategies
Prioritize satiety-promoting foods:
- High protein at every meal (eggs, lean meat, fish, legumes, dairy)
- High fiber foods (vegetables, whole grains, legumes)
- Adequate healthy fats
- Volume eating (large portions of low-calorie foods)
Structure your eating:
- Regular meals (don’t skip, which can lead to overeating)
- Planned snacks if needed
- Avoid grazing or unstructured eating
- Pre-portion foods when possible
Manage your environment:
- Keep challenging foods out of the house
- Stock easy, healthy options
- Make the healthy choice the easy choice
- Reduce exposure to food cues
Exercise for Maintenance
Why exercise matters more now:
- Increases caloric expenditure
- May independently help appetite regulation
- Preserves muscle mass (important for metabolism)
- Provides non-food coping mechanism
Effective approaches:
- Aim for 200+ minutes of moderate activity weekly (more than minimum recommendations)
- Include resistance training 2-3 times weekly
- Find activities you genuinely enjoy
- Build it into your routine as non-negotiable
What research shows:
- Regular exercisers maintain weight better than non-exercisers
- Exercise alone rarely produces weight loss, but it supports maintenance
- The National Weight Control Registry (people who’ve maintained significant loss) shows high rates of physical activity
Behavioral Strategies
Self-monitoring:
- Weigh yourself regularly (daily or weekly)
- Track trends, not individual readings
- Early awareness of regain allows earlier intervention
- Studies show self-weighing predicts better maintenance
Cognitive strategies:
- Recognize hunger vs. appetite vs. habit
- Use delay tactics before eating
- Practice mindful eating
- Address emotional triggers for eating
Environmental management:
- Limit exposure to food cues
- Create friction for overeating
- Establish eating routines and locations
- Manage social situations proactively
Managing the Psychology
Normalizing the difficulty:
- Maintaining weight loss without medication is genuinely hard
- This isn’t a character failing
- Your biology is working against you
- Struggling doesn’t mean you’re doing something wrong
Avoiding all-or-nothing thinking:
- Some regain doesn’t mean you’ve “failed”
- Maintaining most of your loss is still success
- Eating one large meal doesn’t mean the day is ruined
- Progress isn’t linear
Managing expectations:
- Perfect maintenance is unlikely
- Fluctuations are normal
- The goal is a sustainable trajectory, not perfection
Warning Signs and When to Act
Early intervention prevents returning to baseline weight.
Warning Signs of Problematic Regain
Weight patterns to watch:
- Steady upward trend over weeks (not just day-to-day fluctuation)
- Gaining more than 5% of your lowest weight
- Approaching thresholds you predetermined as concerning
Behavioral signs:
- Portion sizes creeping up
- More frequent eating
- Returning to problematic food patterns
- Less structure in eating
- Decreased physical activity
Psychological signs:
- Increased food preoccupation
- Feeling out of control around food
- Emotional eating re-emerging
- Frustration and hopelessness about eating
Action Thresholds
Consider establishing in advance:
5% regain threshold:
- Example: From 187 pounds, concerning at 196 pounds
- Action: Intensify behavioral efforts, increase monitoring
10% regain threshold:
- Example: From 187 pounds, concerning at 206 pounds
- Action: Consider restarting medication, consult with provider
15% regain threshold:
- Example: From 187 pounds, concerning at 215 pounds
- Action: Strongly consider restarting medication
Having predetermined thresholds:
- Removes emotional decision-making in the moment
- Encourages earlier action
- Prevents waiting until you’ve regained everything
When to Consider Restarting
Restarting is appropriate when:
- Weight regain is significant and continuing
- Behavioral efforts aren’t controlling appetite
- Weight-related health conditions are worsening (blood sugar, blood pressure)
- Quality of life is declining
- You want to prevent return to baseline
Restarting isn’t failure:
- It’s appropriate management of a chronic condition
- Many patients stop, try maintaining, and successfully restart
- The medication will work again if you restart
- No shame in needing continued pharmacological support
The Case for Not Stopping
Before deciding to stop, consider the alternative: continued treatment.
Why Many Patients Continue Indefinitely
Reliable maintenance:
- Weight loss is maintained as long as treatment continues
- No need to fight biological forces without support
- Cardiovascular protection continues
- Quality of life preserved
Chronic disease management paradigm:
- Obesity is recognized as a chronic disease
- Chronic diseases typically require ongoing management
- Blood pressure medication isn’t expected to “cure” hypertension
- Weight management medication similarly manages an ongoing condition
Risk-benefit consideration:
- Ongoing medication vs. probable weight regain
- Continued cardiovascular protection vs. returning risk
- Sustained quality of life vs. potential decline
- Known cost vs. unknown health costs of regain
Who Should Consider Continued Treatment
Strong candidates for indefinite treatment:
- Significant weight loss achieved (20%+)
- Weight-related health conditions improved
- History of weight cycling (lose and regain repeatedly)
- Strong biological appetite drivers
- Cardiovascular disease or high risk
- Difficulty maintaining weight loss historically
The decision to continue:
- Doesn’t mean you’ve failed
- Means you’re appropriately managing a chronic condition
- Provides security of maintained results
- Allows you to live without constant food struggle
Making the Decision
Questions to consider:
Why do you want to stop?
- Cost concerns (valid; explore alternatives)
- Side effects (valid; discuss with provider)
- Belief you “should” be able to manage without medication (examine this assumption)
- Dislike of ongoing treatment (understandable, but weigh against alternatives)
What’s your realistic expectation?
- If you stop, what do you think will happen?
- Is that expectation aligned with what research shows?
- Are you prepared for the likely outcomes?
What’s your plan if weight regains?
- Will you restart medication?
- At what point?
- Is the trial of stopping worth the risk?
Is continued treatment actually an option?
- Can you afford ongoing treatment?
- Are there more affordable options (compounded semaglutide)?
- Is the cost of treatment less than the cost of regain (health, quality of life)?
Life After Ozempic: Different Scenarios
Different situations lead to different paths after stopping.
Scenario 1: Planned Discontinuation With Good Outcomes
The best-case scenario:
- Made substantial lifestyle changes during treatment
- Achieved modest, sustainable weight loss
- Eating patterns feel genuinely different, not forced
- Exercise is established routine
- Weight remains stable after stopping (within 5-10% of lowest)
- Maintained vigilance catches any creep early
What this looks like:
- You stop medication and appetite returns but is manageable
- You maintain most of your weight loss through established habits
- Some weight returns but you stabilize at an acceptable level
- Years later, you’re still at a significantly lower weight than baseline
Likelihood: This represents the minority of patients. Possible, especially with modest weight loss goals and genuine lifestyle transformation, but not the typical outcome.
Scenario 2: Gradual Regain and Eventual Restart
The common scenario:
- Stop medication and initially feel okay
- Over months, appetite increases and weight creeps up
- Despite efforts, regain continues
- Eventually restart medication
- Return to previous weight loss with treatment
What this looks like:
- You stop and do well for a few months
- Weight starts increasing at month 3-4
- By month 6-9, you’ve regained significant weight
- You discuss with provider and restart
- Within months of restarting, weight returns to lower level
Perspective: This isn’t failure. It’s appropriate use of medication when needed, discontinuation when desired, and resumption when necessary. Many patients follow this pattern.
Scenario 3: Rapid Regain and Quick Restart
For some patients:
- Appetite returns quickly and intensely
- Weight gain begins within weeks
- Clear that medication is needed
- Restart relatively quickly
What this looks like:
- You stop and immediately notice increased hunger
- Within weeks, eating patterns shift and weight increases
- You recognize this isn’t sustainable
- You restart within 2-3 months
- Weight stabilizes with resumed treatment
Perspective: Quick recognition and action limits regain. Better to restart promptly than wait until baseline weight returns.
Scenario 4: Stop Due to Side Effects or Circumstances
Sometimes stopping isn’t a choice:
- Intolerable side effects require discontinuation
- Medical circumstances (pregnancy planning, surgery)
- Financial constraints make treatment unaffordable
- Access issues prevent continuation
What this looks like:
- You need to stop regardless of preference
- Focus shifts to maintaining what’s possible
- Maximum behavioral efforts applied
- Consider alternatives (other medications, compounded options for cost)
- Realistic expectations about outcomes
Perspective: Do your best with the situation. Some regain is likely, but maintaining even part of your loss is better than the pre-treatment status.
Practical Considerations for Life After Ozempic
Beyond the biology, practical factors affect the post-medication experience.
Cost Considerations
If stopping due to cost:
- Explore all pricing options first
- Compounded semaglutide ($199/month) is significantly less than brand-name
- Manufacturer programs may reduce cost
- Is there any way to make continued treatment affordable?
The cost of regain:
- Increased healthcare costs from weight-related conditions
- Potential medication costs for diabetes, blood pressure, etc.
- Quality of life costs
- Sometimes continued weight medication is cost-effective compared to alternatives
Healthcare Provider Relationship
Maintaining connection:
- Stay in contact with your provider after stopping
- Schedule follow-up to monitor progress
- Don’t disappear and return only after significant regain
- Proactive communication enables earlier intervention
What to discuss:
- Your monitoring plan
- Thresholds for concern
- When to reach out
- Options if weight regains
Emotional Aspects
Common experiences:
- Grief over needing medication
- Frustration at biological reality
- Anxiety about regain
- Self-judgment if weight returns
- Relief if stopping goes well
Healthy perspectives:
- Needing treatment for a chronic condition is normal
- Regain isn’t character failure
- Your worth isn’t determined by the scale
- You’re doing your best with a challenging situation
Social and Lifestyle Factors
Navigating changes:
- Social eating situations may become harder
- Restaurant portions may seem more tempting
- Food-centered gatherings more challenging
- May need new strategies for situations that were easy during treatment
Maintaining support:
- Keep people who supported you during treatment informed
- Don’t isolate if struggling
- Consider support groups or communities
- Professional support (therapist, dietitian) may help
Frequently Asked Questions
What happens when you stop taking Ozempic?
When you stop taking Ozempic, the medication gradually clears from your system over 4-5 weeks, and its effects fade. Most notably, appetite returns to pre-treatment levels or sometimes temporarily higher. The hunger suppression, slowed gastric emptying, and reduced food cravings that the medication provided all reverse. For most patients, this leads to increased food intake and gradual weight regain. Research shows approximately two-thirds of lost weight typically returns within one year of stopping. Blood sugar may also worsen for diabetic patients.
Can you maintain weight loss after stopping Ozempic?
Some patients do maintain significant weight loss after stopping, but they are the minority. Success is more likely for those who achieved modest weight loss (10-15%), made substantial lifestyle changes during treatment, exercise regularly, and whose eating wasn’t primarily driven by biological factors. Most patients experience significant regain regardless of their efforts because the biological drivers of appetite and weight regulation return when the medication stops. The medication was managing these factors, not permanently changing them.
How much weight will I regain after stopping Ozempic?
Research shows patients typically regain approximately two-thirds of their lost weight within one year of stopping. So if you lost 30 pounds, you might expect to regain about 20 pounds. Individual experiences vary—some regain more, some less—but the two-thirds pattern is consistent in studies. The regain happens gradually over months rather than immediately. Some patients regain nearly all lost weight; a minority maintains most of their loss. There’s no way to predict your individual outcome with certainty.
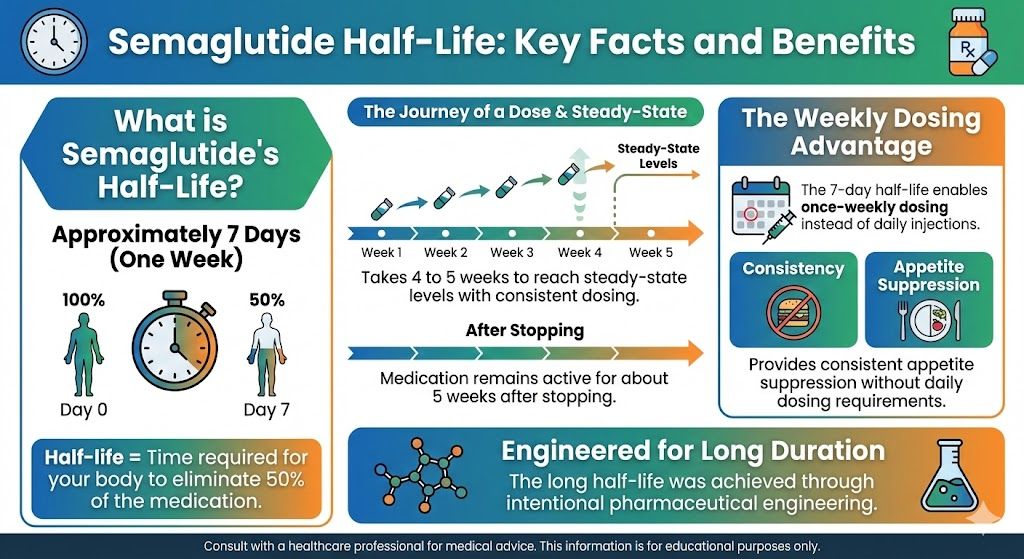
How long do Ozempic effects last after stopping?
The medication has a half-life of about one week, so it takes 4-5 weeks for semaglutide to fully clear your system. During this time, effects gradually diminish. Appetite typically begins returning within the first few weeks after stopping, though you may not notice dramatic changes immediately. By 4-6 weeks after your last dose, most patients notice significantly increased appetite. The full impact on weight becomes apparent over months as eating patterns shift and regain occurs.
Is there a way to prevent weight regain after stopping Ozempic?
There’s no guaranteed way to prevent regain because the biological factors driving weight gain remain when medication stops. However, you can improve your chances by: establishing strong exercise habits (200+ minutes weekly), developing sustainable eating patterns focused on protein and fiber, maintaining vigilant self-monitoring (regular weigh-ins), creating an environment that supports healthy choices, having a plan for early intervention if weight increases, and being willing to restart medication if needed. Even with optimal efforts, significant regain occurs for most patients.
Should I taper off Ozempic or stop suddenly?
Either approach is medically acceptable. There’s no medical requirement to taper, and stopping abruptly doesn’t cause withdrawal or dangerous effects. Some patients prefer gradual reduction for psychological preparation—experiencing the returning appetite incrementally rather than all at once. Others prefer to simply stop. Discuss with your provider which approach makes sense for you. Neither method has been shown to improve long-term maintenance outcomes.
When should I restart Ozempic if I’ve stopped?
Consider restarting when: weight regain becomes significant (typically 10-15% above your lowest weight), behavioral efforts aren’t controlling appetite and weight, weight-related health conditions worsen, or quality of life is declining. Having predetermined thresholds before stopping helps make this decision objectively rather than emotionally. Restarting sooner limits how much weight you regain. There’s no shame in restarting—it’s appropriate management of a chronic condition.
Will Ozempic work again if I restart after stopping?
Yes, semaglutide remains effective if you restart after a period of discontinuation. You’ll follow the standard titration schedule again (starting at lower doses and increasing), and the medication will produce appetite suppression and weight loss as before. Patients who stop, regain, and restart typically return to their previous lower weights with resumed treatment. The medication doesn’t become less effective due to previous use.
Why do I feel so hungry after stopping Ozempic?
The hunger you experience after stopping is your natural appetite regulation reasserting itself. Semaglutide was suppressing appetite by activating GLP-1 receptors in your brain. Without the medication, these receptors return to their baseline activity, and your natural hunger signals resume. Additionally, weight loss causes hormonal changes (increased ghrelin, decreased leptin) that increase hunger. These biological factors were being overridden by the medication; when it stops, they push strongly toward eating more and weight regain.
Is it better to stay on Ozempic long-term or try to stop?
This is a personal decision without a single right answer. Staying on medication long-term provides reliable weight maintenance, continued cardiovascular protection, and freedom from constant appetite management. Stopping allows you to test whether you can maintain independently, reduces ongoing costs, and avoids indefinite medication use. Consider: Why do you want to stop? What are your realistic expectations if you do? Are you prepared for likely regain and willing to restart? For most patients, continued treatment provides more reliable outcomes, but the decision depends on your individual circumstances, values, and goals.
The Bottom Line
Life after Ozempic is possible, but it’s important to enter it with realistic expectations. The medication was managing biological factors that don’t permanently change when treatment stops. For most patients, appetite returns, eating increases, and weight regains—typically about two-thirds of what was lost within a year.
This isn’t a reason to never try stopping if that’s your goal. Some patients do maintain significant weight loss through substantial lifestyle changes, regular exercise, and vigilant monitoring. If you want to try, prepare carefully, have a plan, and be willing to restart if weight regains.
It is, however, a reason to think carefully about whether stopping is the right choice for you. Continued treatment remains an option that reliably maintains results. Needing ongoing medication for a chronic condition isn’t failure—it’s appropriate medical management.
Whatever you decide, understanding the likely outcomes helps you make an informed choice and plan accordingly. If you stop and weight returns, restarting is always available. If you continue treatment, you maintain the benefits you’ve achieved. Either path is valid; the important thing is choosing consciously based on realistic expectations.
Ready to explore semaglutide treatment or restart after discontinuation? TrimRx offers consultations with licensed providers who can evaluate your eligibility and prescribe compounded semaglutide at $199/month for qualifying patients.

Transforming Lives, One Step at a Time
Keep reading
Ozempic for Emotional Eating: Does It Help?
Emotional eating is one of the most common and least discussed barriers to sustainable weight loss. For people who eat in response to stress,…
Hashimoto’s and Ozempic: Safety Considerations
Hashimoto’s thyroiditis is the most common autoimmune condition in the United States, affecting an estimated 14 million people, the majority of them women. It’s…
Ozempic and Anxiety: Side Effects and Interactions (2026)
Anxiety is one of the more nuanced topics that comes up in conversations about GLP-1 medications. Some people report that starting Ozempic worsened their…