Ozempic and Pregnancy: Safety, Risks, and What You Need to Know

If you’re taking Ozempic and wondering about pregnancy—whether you’re planning to conceive, worried you might be pregnant, or wondering about the future—you need clear, accurate information. Maybe your doctor briefly mentioned stopping before pregnancy without explaining the timeline, or perhaps you’re concerned about what happens if you became pregnant while taking the medication.
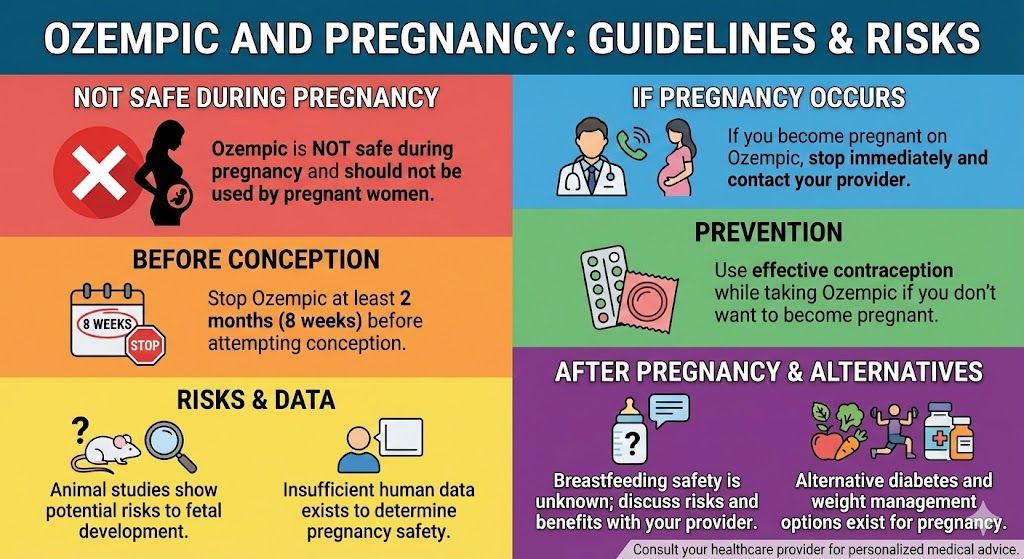
Here’s what you need to know upfront: Ozempic is not safe during pregnancy and you should not take it if you are pregnant or trying to become pregnant.
Animal studies have shown potential risks to fetal development, and there is insufficient human data to determine safety. The official guidance is to stop Ozempic at least 2 months before a planned pregnancy to allow the medication to fully clear your system. If you become pregnant while taking Ozempic, you should stop immediately and contact your healthcare provider. You’ll need alternative approaches to manage diabetes or weight during pregnancy.
This guide provides comprehensive information about Ozempic and pregnancy: why it’s not safe, exactly when to stop before conception, what to do if you’re already pregnant, contraception considerations while taking Ozempic, breastfeeding safety, and planning for pregnancy after treatment.
Key Takeaways: Ozempic and Pregnancy
- Ozempic is NOT safe during pregnancy and should not be used by pregnant women
- Stop Ozempic at least 2 months (8 weeks) before attempting conception
- Animal studies show potential risks to fetal development
- Insufficient human data exists to determine pregnancy safety
- If you become pregnant on Ozempic, stop immediately and contact your provider
- Use effective contraception while taking Ozempic if you don’t want to become pregnant
- Breastfeeding safety is unknown; discuss risks and benefits with your provider
- Alternative diabetes and weight management options exist for pregnancy
The Clear Answer: Ozempic Is Not Safe During Pregnancy
Let’s start with the unambiguous medical guidance: Do not take Ozempic if you are pregnant or planning to become pregnant.
This isn’t a matter of weighing risks and benefits or individual circumstances making it acceptable in some cases. The position is clear across medical organizations and regulatory bodies. The FDA categorizes the risk based on animal study data, and the prescribing information explicitly states that Ozempic should be discontinued at least 2 months before a planned pregnancy.
This guidance exists for several important reasons related to potential fetal harm, lack of adequate human safety data, the long half-life of semaglutide requiring extended washout time, and the availability of safer alternatives for managing diabetes and weight during pregnancy.
Understanding why this guidance exists helps you take it seriously and plan appropriately.
For comprehensive information about Ozempic beyond pregnancy considerations, see our complete guide to Ozempic for weight loss.
Why Ozempic Is Not Safe During Pregnancy
The reasons for avoiding Ozempic during pregnancy are based on animal studies, pharmacological considerations, and the lack of human safety data.
Animal Study Findings
Studies in pregnant rats and rabbits given semaglutide during organogenesis (the critical period when fetal organs develop) showed several concerning findings. Early pregnancy loss increased in animals exposed to semaglutide. Fetal abnormalities occurred at doses similar to or slightly higher than human therapeutic doses. Growth abnormalities were observed in offspring. Structural abnormalities affected various organ systems.
While animal studies don’t perfectly predict human outcomes, they provide crucial early warning signals. When animal studies show potential harm, the precautionary principle applies: avoid use in pregnant humans unless absolutely necessary with no safer alternatives.
Critical Development Periods
Pregnancy involves critical windows where fetal organs develop. The first trimester is particularly crucial for organ formation. Exposure to medications during these windows can disrupt normal development in ways that aren’t reversible.
GLP-1 receptors exist throughout the developing fetus. Activating these receptors pharmacologically during development could theoretically interfere with normal growth and organ maturation processes.
Long Half-Life Considerations
Semaglutide has a half-life of approximately 7 days. This means it takes roughly 5 to 6 weeks (about 5 half-lives) for the medication to be essentially eliminated from your system after your last dose.
If you become pregnant while semaglutide is still in your system, the fetus would be exposed during the critical early development period. This is why stopping 2 months before planned conception is recommended—it ensures complete medication clearance before pregnancy begins.
Lack of Adequate Human Data
There are no adequate and well-controlled studies of semaglutide in pregnant women. The human data that exists comes from inadvertent exposures (women who became pregnant while taking the medication) and post-marketing reports, which are insufficient to establish safety.
Without systematic human studies, we simply don’t know the true risk profile. The absence of data showing harm is not the same as data showing safety. Given the availability of alternatives, exposing pregnant women and fetuses to this uncertainty is not justified.
Effects on Maternal Metabolism
Pregnancy involves significant metabolic changes. Blood sugar regulation, insulin sensitivity, nutrient partitioning, and hormone levels all shift dramatically. Adding a medication that powerfully affects these systems could create unpredictable interactions.
Additionally, many women experience severe nausea and vomiting during early pregnancy (morning sickness). Adding a medication known to cause nausea and vomiting could worsen this significantly, potentially leading to hyperemesis gravidarum (severe pregnancy-related vomiting requiring medical intervention).
When to Stop Ozempic Before Trying to Conceive
If you’re planning to become pregnant, timing is crucial.
The Official Recommendation: 2 Months Before
The FDA and prescribing information recommend stopping Ozempic at least 2 months (8 weeks) before a planned pregnancy. This washout period ensures the medication is completely eliminated from your system before conception occurs.
The 2-month timeline is based on semaglutide’s pharmacokinetics. With a 7-day half-life, 5 half-lives (35 days or about 5 weeks) achieves 97% elimination. The 8-week recommendation provides additional safety margin beyond complete elimination.
Why the Full Washout Period Matters
You might be tempted to shorten this timeline, especially if you’re eager to conceive. However, the full 2-month washout is important because early pregnancy development is so critical. Many women don’t know they’re pregnant until 4 to 6 weeks after conception. If you conceive shortly after stopping Ozempic, residual medication could expose the embryo during crucial early development. The 2-month clearance ensures that by the time you conceive, no medication remains in your system.
Planning Your Timeline
If you’re currently taking Ozempic and want to become pregnant, work backward from your desired conception timeframe. If you want to start trying to conceive in June, you should take your last Ozempic dose no later than early April. If you want to start trying in December, your last dose should be no later than early October.
Mark your calendar clearly. Set reminders. Communicate the timeline to your partner. This planning helps ensure you don’t accidentally conceive too soon after stopping.
What If You’re Not Sure About Timing?
Some women aren’t actively “trying” to conceive but also aren’t preventing pregnancy. If this describes your situation and you’re taking Ozempic, you need to make a clear decision. Either use reliable contraception while on Ozempic or stop Ozempic now to allow the 2-month washout period before any potential pregnancy.
The middle ground—taking Ozempic while not preventing pregnancy—creates unacceptable risk.
Discussing Plans with Your Provider
Before stopping Ozempic in preparation for pregnancy, discuss your plans with your healthcare provider. If you’re taking Ozempic for diabetes management, you’ll need an alternative plan for glucose control during the washout period and pregnancy. If you’re taking it for weight loss, discuss whether continued weight loss efforts before conception make sense or whether maintaining your current weight is a better goal.
Your provider can help you transition off Ozempic safely and put appropriate alternatives in place.
What to Do If You’re Already Pregnant
If you discover you’re pregnant while taking Ozempic, don’t panic but do act quickly.
Stop Immediately
As soon as you have a positive pregnancy test, stop taking Ozempic immediately. Don’t wait for your next scheduled dose or your next doctor’s appointment. Stop now.
Missing doses of Ozempic won’t cause immediate problems. The medication is for chronic management, not acute treatment. Stopping abruptly is safe and appropriate when pregnancy is discovered.
Contact Your Healthcare Provider Right Away
Call your doctor or OB/GYN as soon as possible after confirming pregnancy. Explain that you’ve been taking Ozempic and just discovered you’re pregnant. They need this information to provide appropriate prenatal care.
Don’t delay this call out of embarrassment or worry about being judged. Your healthcare providers need complete information to care for you and your developing baby properly.
Provide Detailed Information
When you speak with your provider, be prepared to share when you took your last dose of Ozempic, what dose you were taking (0.25 mg, 0.5 mg, 1 mg, or 2 mg weekly), how long you’ve been taking it, approximately when conception likely occurred based on your last menstrual period, and whether you’re taking Ozempic for diabetes or weight loss.
This information helps your provider assess the likely level and timing of fetal exposure.
Expect Early Monitoring
Your provider will likely recommend early ultrasound monitoring to date the pregnancy accurately and assess early development. Depending on timing of exposure, additional monitoring throughout pregnancy might be recommended. Your provider might consult with maternal-fetal medicine specialists if there are concerns.
This doesn’t mean something is definitely wrong. Early monitoring is precautionary and helps ensure the best possible outcomes.
Don’t Assume the Worst
While Ozempic shouldn’t be used during pregnancy, accidental exposure in early pregnancy doesn’t mean your baby will definitely have problems. Many women have inadvertently taken medications in early pregnancy before realizing they were pregnant, and most pregnancies turn out fine.
The animal study findings show increased risk, but many exposed animals had normal offspring. The lack of human data means we don’t know the precise risk level. Your individual situation may well result in a completely healthy pregnancy and baby.
Stay positive but vigilant. Follow your provider’s recommendations for monitoring closely.
Alternative Management Plans
If you were taking Ozempic for type 2 diabetes, you’ll need an alternative glucose management plan immediately. Options include insulin (safe during pregnancy), certain oral medications considered acceptable during pregnancy (like metformin in some cases), dietary management, and close glucose monitoring.
If you were taking Ozempic for weight loss, weight management during pregnancy shifts focus. Pregnancy is not a time for weight loss (except in rare circumstances under close medical supervision). Focus shifts to appropriate pregnancy weight gain based on your starting BMI, balanced nutrition to support fetal development, and maintaining activity as appropriate for pregnancy.
Your provider will help you transition to appropriate pregnancy-compatible management approaches.
Contraception While Taking Ozempic
If you’re taking Ozempic and don’t want to become pregnant, reliable contraception is essential.
Why Contraception Matters
Ozempic is used primarily by women of childbearing age for weight loss or diabetes management. Many women taking Ozempic are sexually active and could become pregnant if not using contraception. Given that Ozempic is not safe during pregnancy, preventing unintended pregnancy while taking the medication is crucial.
Additionally, weight loss from Ozempic can affect fertility. Women with polycystic ovary syndrome (PCOS) or obesity-related infertility often experience improved fertility as they lose weight. You might become pregnant more easily than before Ozempic, even if you’ve struggled with infertility previously.
Effective Contraception Options
Discuss contraception with your provider when starting Ozempic. Effective options include long-acting reversible contraceptives (IUDs and implants), which are highly effective and don’t require daily compliance. Birth control pills are effective when taken consistently. Barrier methods (condoms) are moderately effective, especially when combined with other methods. Injectable contraceptives (Depo-Provera) work well for many women.
The most important factor is choosing a method you’ll actually use consistently and correctly.
Consider What Happens If Contraception Fails
No contraception method is 100% effective. Even with perfect use, some pregnancies occur. If you’re taking Ozempic, have a plan for what you’ll do if contraception fails and you become pregnant. Know when to take pregnancy tests (at the first sign of a missed period). Have your provider’s contact information readily available. Understand that you’ll need to stop Ozempic immediately.
This preparation helps you act quickly if needed.
Temporary Contraception During Washout
Remember that you need to continue using contraception during the 2-month washout period after stopping Ozempic. Some couples make the mistake of stopping contraception as soon as they stop Ozempic, not realizing medication is still in the system.
Don’t begin trying to conceive until the full 8 weeks after your last Ozempic dose have passed.
For information about managing weight and health before pregnancy, see our comprehensive semaglutide weight loss guide.
Breastfeeding Considerations
If you’re breastfeeding or planning to breastfeed, you need to know about Ozempic’s safety during lactation.
Limited Safety Data
There is minimal data on semaglutide levels in human breast milk or its effects on breastfed infants. Animal studies show that semaglutide is present in milk of lactating rats at low levels. However, animal milk composition differs significantly from human milk, limiting the applicability of these findings.
Without adequate human data, the safety profile for breastfeeding infants is unknown.
Theoretical Considerations
Semaglutide is a large peptide molecule. Large molecules are generally poorly absorbed from the infant’s digestive tract, potentially limiting systemic exposure even if present in breast milk. Additionally, any semaglutide that reaches the infant’s stomach would likely be broken down by digestive enzymes.
These factors suggest that infant exposure might be minimal even if semaglutide is present in breast milk. However, this remains theoretical without actual data.
The Risk-Benefit Discussion
The decision about taking Ozempic while breastfeeding requires weighing several factors: the importance of breastfeeding for infant health, the mother’s need for Ozempic (diabetes management versus weight loss), availability of alternative treatments, the infant’s age (newborns versus older infants), and individual family circumstances and preferences.
This is not a decision to make independently. Have a detailed discussion with both your OB/GYN and pediatrician.
Most Conservative Approach
The most conservative approach is avoiding Ozempic while breastfeeding, particularly during the first 6 months when breast milk is the sole or primary nutrition source. Consider waiting until after weaning to resume Ozempic for weight loss. Use alternative diabetes management approaches if taking Ozempic primarily for glucose control.
If You Choose to Use Ozempic While Breastfeeding
If you and your providers decide that the benefits of Ozempic outweigh the unknown risks, consider these precautions. Monitor your infant closely for any signs of feeding problems, growth issues, or unusual symptoms. Ensure your infant is having adequate wet diapers and weight gain. Have regular pediatric follow-ups to monitor infant growth and development. Be prepared to stop Ozempic if any concerns arise.
This should be done only under close medical supervision with full informed consent about the unknowns.
Diabetes Management During Pregnancy Without Ozempic
If you were taking Ozempic for diabetes management, pregnancy requires a different approach.
Glucose Control Goals in Pregnancy
Pregnancy requires tight glucose control to prevent complications. Target ranges are more stringent than in non-pregnant individuals. Fasting glucose should be below 95 mg/dL. One-hour post-meal glucose should be below 140 mg/dL. Two-hour post-meal glucose should be below 120 mg/dL.
These tight targets protect both mother and baby from complications of poorly controlled diabetes during pregnancy.
Insulin Is the Gold Standard
Insulin is considered the safest and most effective medication for managing diabetes during pregnancy. It doesn’t cross the placenta, so it doesn’t directly affect the baby. Multiple formulations (rapid-acting, long-acting) allow flexible dosing. Dosing can be adjusted precisely to meet changing needs throughout pregnancy.
Many women who managed diabetes with oral medications or GLP-1 agonists before pregnancy transition to insulin during pregnancy.
Other Medication Options
Some providers use metformin during pregnancy, though it’s not FDA-approved for this use. Metformin does cross the placenta, but extensive use suggests it’s reasonably safe. Glyburide is sometimes used for gestational diabetes, though insulin is generally preferred.
Your endocrinologist or maternal-fetal medicine specialist will help determine the best approach for your specific situation.
Dietary Management
Diet plays a crucial role in managing diabetes during pregnancy. Work with a registered dietitian who specializes in diabetes and pregnancy. Focus on complex carbohydrates with adequate fiber, lean proteins, healthy fats, and frequent small meals to maintain stable blood sugar.
Many women find that dietary changes alone, or combined with insulin, effectively control glucose during pregnancy.
Frequent Monitoring
Pregnancy requires more intensive diabetes monitoring than you might be used to. Check blood sugar multiple times daily (typically 4 to 7 times). Keep detailed logs of readings and food intake. Attend frequent prenatal appointments (often weekly or biweekly in later pregnancy). Adjust medications frequently as pregnancy progresses and insulin resistance changes.
This intensive management helps ensure the best outcomes for you and your baby.
Weight Management During Pregnancy After Ozempic
If you were taking Ozempic primarily for weight loss, pregnancy changes your weight management approach.
Pregnancy Is Not a Time for Weight Loss
With rare exceptions (women with very high BMI under close medical supervision), pregnancy is not an appropriate time to pursue weight loss. Weight loss during pregnancy can deprive the developing fetus of essential nutrients. Even for women with obesity, some weight gain during pregnancy is typically recommended.
Focus shifts from losing weight to appropriate pregnancy weight gain.
Recommended Pregnancy Weight Gain
Recommendations vary based on your pre-pregnancy BMI. For women with BMI under 18.5 (underweight), gain 28 to 40 pounds. For women with BMI 18.5 to 24.9 (normal weight), gain 25 to 35 pounds. For women with BMI 25 to 29.9 (overweight), gain 15 to 25 pounds. For women with BMI over 30 (obesity), gain 11 to 20 pounds.
These are general guidelines. Your provider will give personalized recommendations.
Maintaining Healthy Habits
Focus on healthy behaviors rather than weight loss. Eat balanced, nutritious meals emphasizing vegetables, fruits, whole grains, lean proteins, and healthy fats. Stay physically active with pregnancy-appropriate exercise (walking, swimming, prenatal yoga). Avoid excessive empty calories while meeting increased caloric needs (typically 300 to 500 extra calories daily in second and third trimesters). Listen to hunger and fullness cues without obsessing about weight.
These habits support healthy pregnancy regardless of starting weight.
Managing Concerns About Weight Gain
If you’ve worked hard to lose weight on Ozempic, the thought of gaining weight during pregnancy might cause anxiety. This is understandable but important to reframe. Pregnancy weight gain is normal, necessary, and expected. It supports fetal growth and development. Most pregnancy weight is baby, placenta, amniotic fluid, increased blood volume, and breast tissue—not fat. You can return to weight management after pregnancy and breastfeeding.
Discuss concerns with your provider or a mental health professional if anxiety about pregnancy weight gain becomes overwhelming.
Planning for Pregnancy After Ozempic Treatment
If you’re considering using Ozempic before pregnancy with a plan to conceive after reaching your weight goals, strategic planning helps.
Achieving Goal Weight Before Conception
Many women want to lose weight before pregnancy for several good reasons. Lower pre-pregnancy weight reduces risks of gestational diabetes, preeclampsia, C-section, and complications. Improved metabolic health before conception benefits pregnancy outcomes. Starting pregnancy at a healthier weight makes pregnancy physically easier.
Using Ozempic to achieve significant weight loss before pregnancy can be a reasonable strategy if you allow appropriate washout time.
Build in Extra Time
When planning your timeline, build in cushion time beyond the minimum 2-month washout. Life doesn’t always go according to plan. Conception might take longer than expected. You might want to maintain your new weight for a while before pregnancy. Having flexibility reduces stress and pressure.
Consider stopping Ozempic when you’re 3 to 6 months away from wanting to start trying to conceive rather than cutting it as close as possible to the 2-month minimum.
Maintenance Strategies
After stopping Ozempic, you’ll need strategies to maintain your weight loss during the washout period and pregnancy planning phase. Focus on continuing healthy eating patterns you developed during treatment. Maintain regular physical activity. Consider working with a registered dietitian for ongoing support. Address any emotional or behavioral factors that contributed to weight gain originally. Build sustainable habits that don’t depend on medication.
Many people find that the months on Ozempic helped them develop better habits that support maintenance after stopping.
Consider Your Overall Health Picture
Before pregnancy, address any health issues beyond just weight. Achieve good glucose control if you have diabetes or prediabetes. Optimize blood pressure. Address nutritional deficiencies (take prenatal vitamins with folic acid before conception). Stop smoking if applicable. Reduce alcohol consumption. Achieve the healthiest possible baseline before conceiving.
These factors affect pregnancy outcomes as much as or more than weight.
Work with Your Healthcare Team
Involve your OB/GYN, endocrinologist (if you have diabetes), and potentially a maternal-fetal medicine specialist in your planning. They can help optimize your health before conception, guide the transition off Ozempic, support weight maintenance strategies, and provide preconception counseling.
This team approach helps ensure the healthiest possible pregnancy when you’re ready.
For information about stopping Ozempic, see our guide to how long semaglutide stays in your system.
Comparing Pregnancy Guidelines Across GLP-1 Medications
Understanding whether other GLP-1 medications have different pregnancy safety profiles might be relevant.
All GLP-1 Medications Have Similar Warnings
Semaglutide (Ozempic, Wegovy), tirzepatide (Mounjaro, Zepbound), liraglutide (Victoza, Saxenda), and dulaglutide (Trulicity) all carry warnings against use during pregnancy. The recommendations are consistent across the class. Stop 2 months before planned pregnancy. Don’t use during pregnancy. Unknown safety during breastfeeding.
This consistency reflects the shared mechanism of action and similar concerns about fetal exposure.
Don’t Assume One Is Safer
No GLP-1 medication is considered safe during pregnancy. Don’t switch from one to another thinking it might be acceptable to continue. If you’re planning pregnancy, all GLP-1 medications should be discontinued with appropriate washout time.
Other Diabetes Medications in Pregnancy
If you need diabetes management during pregnancy, medications considered safer include insulin (first-line, safest option), metformin (used by some providers though technically off-label), and glyburide (sometimes used for gestational diabetes).
Discuss options with your endocrinologist and maternal-fetal medicine specialist.
Frequently Asked Questions
Can you take Ozempic while pregnant?
No. Ozempic is not safe during pregnancy and should not be used by pregnant women. Animal studies show potential risks to fetal development, and there is insufficient human data to determine safety. If you are pregnant or planning to become pregnant, do not take Ozempic. If you become pregnant while taking Ozempic, stop immediately and contact your healthcare provider.
How long before pregnancy should you stop Ozempic?
Stop Ozempic at least 2 months (8 weeks) before trying to conceive. This washout period ensures the medication is completely eliminated from your system before pregnancy begins. Semaglutide has a 7-day half-life, and it takes approximately 5 weeks for 97% elimination. The 2-month recommendation provides additional safety margin. Don’t attempt to conceive until this full washout period has passed.
What happens if you get pregnant while on Ozempic?
If you discover you’re pregnant while taking Ozempic, stop the medication immediately and contact your healthcare provider right away. Don’t wait for your next scheduled dose or appointment. Your provider will likely recommend early ultrasound monitoring and may consult with maternal-fetal medicine specialists. While accidental exposure doesn’t guarantee harm to the baby, close monitoring throughout pregnancy is important.
Can Ozempic cause birth defects?
Animal studies showed increased risks of pregnancy loss, fetal abnormalities, and growth issues at doses similar to human therapeutic levels. However, adequate human studies don’t exist to definitively determine the risk and types of birth defects in humans. Due to this uncertainty and the concerning animal data, Ozempic should not be used during pregnancy. The potential risks are serious enough to warrant complete avoidance.
Is Ozempic safe while breastfeeding?
The safety of Ozempic during breastfeeding is unknown. There is insufficient data on semaglutide levels in human breast milk or effects on breastfed infants. The most conservative approach is to avoid Ozempic while breastfeeding, particularly during the first 6 months when breast milk is the primary nutrition source. If considering Ozempic while breastfeeding, discuss the unknown risks and potential benefits thoroughly with your OB/GYN and pediatrician.
Can Ozempic affect fertility?
Ozempic doesn’t directly impair fertility, but weight loss from the medication can actually improve fertility, particularly in women with PCOS or obesity-related infertility. As you lose weight, ovulation may become more regular and conception easier. If you’re taking Ozempic and don’t want to become pregnant, use reliable contraception because you may be more fertile than before starting treatment.
What diabetes medication is safe during pregnancy?
Insulin is considered the safest and most effective medication for managing diabetes during pregnancy. It doesn’t cross the placenta and can be adjusted precisely to meet changing needs throughout pregnancy. Some providers also use metformin or glyburide during pregnancy, though these are less preferred than insulin. Discuss the best options for your specific situation with your endocrinologist and maternal-fetal medicine specialist.
Can you lose weight during pregnancy?
Generally, no. Pregnancy is not an appropriate time to pursue weight loss except in rare circumstances under close medical supervision for women with very high BMI. Even women with obesity are typically advised to gain some weight during pregnancy (usually 11 to 20 pounds). Weight loss during pregnancy can deprive the developing fetus of essential nutrients. Focus on healthy eating and appropriate pregnancy weight gain rather than weight loss.
How soon can you start Ozempic after giving birth?
If you’re not breastfeeding, you can typically restart Ozempic after your postpartum checkup (usually 6 weeks after delivery) once your provider confirms you’ve recovered well from childbirth. If you’re breastfeeding, the safety is unknown, and the most conservative approach is waiting until after weaning to resume Ozempic. Discuss the timing with your OB/GYN and consider your individual circumstances, health needs, and infant feeding plans.
What should I do if I took Ozempic before knowing I was pregnant?
Stop taking Ozempic immediately upon discovering you’re pregnant. Contact your healthcare provider right away to inform them of the exposure. Don’t panic—many accidental medication exposures in early pregnancy result in healthy babies, but your provider needs this information to provide appropriate prenatal care and monitoring. Follow your provider’s recommendations for any additional testing or monitoring throughout your pregnancy.
Making Informed Decisions About Ozempic and Pregnancy
The relationship between Ozempic and pregnancy is straightforward: the medication should not be used during pregnancy or within 2 months of planned conception due to potential fetal risks demonstrated in animal studies and lack of adequate human safety data. This clear guidance helps protect both maternal and fetal health while allowing women to plan appropriately for pregnancy if desired.
If you’re taking Ozempic and planning to become pregnant, stopping at least 2 months before conception attempts, using reliable contraception until the washout period is complete, and working with your healthcare team to develop alternative management plans for diabetes or weight gives you the best foundation for a healthy pregnancy.
If you discover you’re pregnant while taking Ozempic, immediately stopping the medication and promptly contacting your provider for appropriate monitoring and care helps ensure the best possible outcomes despite the accidental exposure.
The key is informed planning and open communication with your healthcare team. Whether you’re actively planning pregnancy, want to keep your options open for the future, or need to prevent pregnancy while pursuing weight loss goals, understanding how Ozempic affects these considerations helps you make decisions aligned with your health priorities and family planning goals.
Whether you’re using brand-name Ozempic or more affordable compounded semaglutide at $199 monthly through TrimRx, the pregnancy considerations remain identical. Get started with comprehensive medical support and guidance that includes appropriate family planning counseling, ensuring you can pursue your health goals while protecting your reproductive health and any future pregnancies.

Transforming Lives, One Step at a Time
Keep reading
Online Ozempic Prescription Texas
You can get an Ozempic prescription online in Texas through a licensed telehealth provider without an in-person visit. Texas telehealth law allows providers to…
Online Ozempic Prescription California
You can get an Ozempic prescription online in California through a licensed telehealth provider without an in-person visit. California’s telehealth laws allow providers to…
Weight Loss Clinic Online Texas: Your Options
An online weight loss clinic in Texas gives you access to GLP-1 medications like semaglutide and tirzepatide through a fully virtual process. You complete…



