Ozempic BMI Requirements: Do You Qualify for Treatment?

You’ve heard about the results people are getting with Ozempic and you want to know if you qualify. The first question most people ask is about BMI: What number do you need to hit? Is there a hard cutoff? And what happens if you’re close but not quite there?
The answer is more nuanced than a single number, but here’s the straightforward version: For weight loss treatment with semaglutide (the active ingredient in Ozempic and Wegovy), the standard eligibility threshold is a BMI of 30 or higher. If your BMI falls between 27 and 30, you can still qualify if you have at least one weight-related health condition like high blood pressure, Type 2 diabetes, or high cholesterol.
These thresholds come from FDA approval criteria for Wegovy (the weight loss version of semaglutide) and have become the standard that most prescribers follow, even when prescribing Ozempic off-label. Understanding exactly how these requirements work, what conditions count as qualifiers, and what options exist if you’re borderline helps you navigate the process more effectively.
This guide covers:
- The specific BMI thresholds for semaglutide eligibility
- How to calculate your BMI accurately
- Which weight-related health conditions qualify you at lower BMI levels
- The difference between Ozempic and Wegovy eligibility
- What to do if you’re close to but below the threshold
- How different prescribers interpret the requirements
- Insurance versus cash-pay eligibility differences
- Common situations and whether they qualify
Key Takeaways
- BMI 30 or higher qualifies you for semaglutide treatment for weight management, regardless of other health conditions
- BMI 27-29.9 qualifies you if you have at least one weight-related health condition (hypertension, Type 2 diabetes, dyslipidemia, sleep apnea, etc.)
- BMI below 27 typically does not qualify for semaglutide prescriptions, even with health conditions
- Ozempic is FDA-approved for Type 2 diabetes, not weight loss, so its “official” eligibility is different from practical prescribing
- Wegovy uses the BMI 30/27 thresholds as its FDA-approved indication for chronic weight management
- Most prescribers follow Wegovy’s criteria even when prescribing Ozempic off-label for weight loss
- BMI calculations use height and weight only and don’t account for muscle mass, body composition, or fat distribution
- Insurance companies apply stricter criteria than cash-pay options, often requiring documented failed attempts at other treatments
- Telehealth platforms generally follow standard criteria but evaluate each patient individually
- Borderline cases may qualify after evaluation reveals previously undiagnosed conditions like prediabetes or fatty liver
Understanding BMI and How It’s Calculated
Before diving into specific requirements, it’s worth understanding what BMI actually measures and how to calculate yours accurately.
BMI stands for Body Mass Index, a simple ratio of weight to height that provides a rough estimate of body fatness. It was developed in the 1800s as a population-level statistical tool and has since become the standard screening metric for weight classification in clinical settings.
The formula for BMI is weight in kilograms divided by height in meters squared. For those using pounds and inches (which is most Americans), the formula is weight in pounds divided by height in inches squared, multiplied by 703.
Here’s the practical calculation: Take your weight in pounds. Divide it by your height in inches. Divide by your height in inches again. Multiply by 703. The result is your BMI.
For example, someone who weighs 200 pounds and stands 5’8″ (68 inches) would calculate: 200 ÷ 68 ÷ 68 × 703 = 30.4 BMI.
You don’t need to do this math yourself. Any online BMI calculator will give you the number instantly. Just make sure you’re using accurate, recent measurements. Your weight from your last doctor’s visit six months ago may not reflect your current situation.
BMI Categories
The standard BMI categories used in clinical practice are:
| BMI Range | Classification |
| Below 18.5 | Underweight |
| 18.5 to 24.9 | Normal weight |
| 25 to 29.9 | Overweight |
| 30 to 34.9 | Obesity Class I |
| 35 to 39.9 | Obesity Class II |
| 40 and above | Obesity Class III |
For semaglutide eligibility, the key thresholds are 27 (the lower bound with qualifying conditions) and 30 (qualifies without additional conditions).
Limitations of BMI
BMI is a useful screening tool but an imperfect one. It measures weight relative to height without distinguishing between muscle and fat. A muscular athlete and an inactive person with high body fat can have identical BMIs despite very different health profiles.
BMI also doesn’t account for where fat is distributed on the body. Visceral fat (around the organs in the midsection) poses greater health risks than subcutaneous fat (under the skin in other areas). Two people with the same BMI but different fat distribution patterns face different health risks.
Additionally, BMI thresholds were developed primarily using data from white European populations and may not be equally applicable across all ethnicities. Some research suggests that health risks associated with higher BMI may occur at lower thresholds for certain populations, including people of Asian descent.
Despite these limitations, BMI remains the standard clinical metric because it’s simple, inexpensive, and correlates reasonably well with health outcomes at the population level. Prescribers use it as a starting point for eligibility assessment, not as the sole determining factor.
The Official BMI Requirements for Semaglutide
Now let’s get specific about what the actual requirements are and where they come from.
Wegovy (Semaglutide for Weight Loss) FDA Criteria
Wegovy received FDA approval in June 2021 specifically for chronic weight management. The approved indication specifies that Wegovy is for adults with:
- BMI of 30 kg/m² or greater (obesity), OR
- BMI of 27 kg/m² or greater (overweight) with at least one weight-related comorbidity
Weight-related comorbidities specified in the approval include hypertension, Type 2 diabetes, and dyslipidemia (abnormal cholesterol or triglyceride levels).
These criteria form the foundation for how most prescribers evaluate patients for semaglutide treatment for weight loss, regardless of whether they’re prescribing brand-name Wegovy, off-label Ozempic, or compounded semaglutide.
Ozempic (Semaglutide for Diabetes) FDA Criteria
Ozempic’s FDA approval is different because it’s approved for Type 2 diabetes, not weight loss. The official indication is for improving glycemic control in adults with Type 2 diabetes as an adjunct to diet and exercise.
Technically, there are no BMI requirements for Ozempic’s approved use. If you have Type 2 diabetes, your doctor can prescribe Ozempic regardless of your weight. The medication helps control blood sugar, and weight loss is essentially a beneficial side effect.
However, when doctors prescribe Ozempic off-label specifically for weight loss (rather than diabetes management), they typically apply the same BMI criteria used for Wegovy. This makes clinical sense since the medication, dose, and intended effect are essentially the same.
For more details on the full range of eligibility factors beyond BMI, see our guide on who qualifies for Ozempic.
Why the BMI 30/27 Thresholds Exist
The specific BMI thresholds aren’t arbitrary. They’re based on epidemiological data about when excess weight begins causing measurable health consequences and when the benefits of pharmacological intervention outweigh the risks.
At a BMI of 30 and above, the statistical risks of conditions like Type 2 diabetes, cardiovascular disease, certain cancers, and premature death increase substantially. The medical consensus is that this level of excess weight constitutes a disease state (obesity) warranting treatment.
Between BMI 27 and 30, the picture is more mixed. Some people in this range are metabolically healthy with few weight-related issues. Others have significant health impacts. The additional requirement for a weight-related condition helps identify which overweight individuals would benefit most from medication.
Below BMI 27, the risk-benefit calculation generally doesn’t favor semaglutide treatment. The medication has real side effects and costs, and for people who are only modestly overweight without health complications, the potential benefits don’t clearly outweigh these drawbacks.
Weight-Related Conditions That Qualify You at Lower BMI
If your BMI falls between 27 and 29.9, you need at least one weight-related health condition to qualify. Understanding which conditions count helps you assess your eligibility and prepare for discussions with prescribers.
Conditions That Definitely Qualify
Type 2 Diabetes: This is the most straightforward qualifier since semaglutide was originally developed as a diabetes medication. If you have diagnosed Type 2 diabetes, you qualify at BMI 27+ (and can get Ozempic for the diabetes itself regardless of BMI).
Prediabetes: Elevated blood sugar that hasn’t yet reached diabetic levels also qualifies. Prediabetes is defined as fasting glucose between 100-125 mg/dL or HbA1c between 5.7-6.4%. Many people have prediabetes without knowing it, which is why bloodwork before prescribing can be valuable.
Hypertension (High Blood Pressure): Blood pressure consistently at or above 130/80 mmHg qualifies as hypertension. If you take blood pressure medication, you have documented hypertension even if your current readings are controlled.
Dyslipidemia: This includes high LDL cholesterol, low HDL cholesterol, or high triglycerides. If you take statins or other cholesterol medications, you have documented dyslipidemia.
Obstructive Sleep Apnea: Diagnosed OSA, especially if you use a CPAP machine, qualifies. Sleep apnea is strongly associated with excess weight and often improves significantly with weight loss.
Cardiovascular Disease: History of heart attack, stroke, angina, heart failure, or other cardiovascular conditions qualifies you. These conditions make weight management particularly important.
Conditions That Typically Qualify
Non-Alcoholic Fatty Liver Disease (NAFLD): Fat accumulation in the liver is increasingly common and strongly associated with excess weight. Diagnosed NAFLD typically qualifies you for treatment.
Polycystic Ovary Syndrome (PCOS): This hormonal condition is closely linked to weight and insulin resistance. Women with PCOS often qualify for semaglutide at lower BMI thresholds.
Osteoarthritis: Particularly in weight-bearing joints like knees and hips, osteoarthritis is exacerbated by excess weight. If you have documented joint disease, this may qualify you.
Gastroesophageal Reflux Disease (GERD): Chronic acid reflux is often weight-related and may serve as a qualifying condition, though this varies by prescriber.
How These Conditions Are Documented
Having a qualifying condition means having it documented in your medical records. A self-reported belief that you have high blood pressure isn’t sufficient. You need either a formal diagnosis, documented measurements meeting diagnostic criteria, or evidence of treatment (such as being on blood pressure medication).
If you believe you have a qualifying condition but it hasn’t been formally diagnosed, discuss this with your doctor. They may want to run tests to confirm. Sometimes this process reveals conditions you didn’t know you had, which can actually help your eligibility case.
For example, routine bloodwork might show your fasting glucose is 108 mg/dL, which is prediabetes. You didn’t know you had it, but now it’s documented and serves as a qualifying condition for semaglutide at BMI 27+.
How Different Prescribers Apply BMI Requirements
While the BMI 30/27 thresholds are standard, how strictly different prescribers apply them varies somewhat. Understanding these variations helps you navigate the process.
Primary Care Physicians
Primary care doctors are often the first stop for patients interested in semaglutide. Their approach to BMI requirements varies based on their familiarity with these medications and their overall philosophy about weight management.
Some primary care physicians follow the thresholds strictly, requiring documented BMI and qualifying conditions before prescribing. Others take a more holistic view, considering factors beyond raw BMI numbers. A patient at BMI 29 with clear health impacts from their weight might get different consideration than a patient at BMI 31 who’s metabolically healthy.
Primary care doctors also vary in their willingness to prescribe semaglutide at all. Some prescribe routinely, while others prefer referring to specialists. If your PCP seems hesitant, it may be more about their comfort with the medication than your specific eligibility.
Endocrinologists and Obesity Medicine Specialists
Specialists in endocrinology and obesity medicine prescribe semaglutide frequently and tend to be more sophisticated in their eligibility assessments. They understand the limitations of BMI as a metric and may consider additional factors like waist circumference, body composition, metabolic markers, and individual health trajectory.
A specialist might be more willing to prescribe for a borderline patient if other factors suggest they’d benefit. They also have more experience identifying qualifying conditions that patients may not have realized they have.
The trade-off is that specialists often have longer wait times for appointments and may cost more than primary care visits. But if you’re borderline on eligibility, a specialist evaluation might be worthwhile.
Telehealth Platforms
Telehealth platforms that prescribe semaglutide generally follow standard BMI criteria but vary in how they apply them. Most require patients to self-report height and weight, which is then used to calculate BMI. Some may request verification through photos or recent medical records.
Reputable telehealth platforms like TrimRx evaluate each patient individually, considering BMI alongside health history and qualifying conditions. The consultation process is designed to determine whether treatment is appropriate for your specific situation.
Telehealth can be particularly accessible for patients who face barriers with traditional healthcare, whether due to location, availability, cost, or discomfort discussing weight in person. For guidance on the telehealth prescription process, see our article on how to get prescribed Ozempic.
Weight Loss Clinics
Medical weight loss clinics specialize in helping patients lose weight through various interventions, including medication. Their eligibility assessments tend to be thorough, and they’re experienced at identifying qualifying conditions.
Some clinics have their own protocols that may be slightly more or less restrictive than standard thresholds. They may also bundle medication with program fees, assessments, and ongoing monitoring, which affects overall cost but can provide more comprehensive support.
Insurance Requirements vs. Cash-Pay Requirements
An important distinction exists between what’s medically appropriate (what doctors are willing to prescribe) and what insurance will cover. These aren’t always the same.
Insurance Prior Authorization Requirements
When you try to get semaglutide covered by insurance, the insurance company applies its own eligibility criteria, which are often stricter than medical prescribing standards.
Common insurance requirements beyond basic BMI thresholds include:
Documentation of previous weight loss attempts: Many insurers require evidence that you’ve tried diet, exercise, or other weight loss methods before approving medication. This might mean documented participation in a weight loss program, records of working with a nutritionist, or a certain period of physician-supervised lifestyle modification.
Specific BMI documentation: Insurance companies typically require recent, clinically measured BMI rather than self-reported numbers. Your doctor’s office may need to submit records of your weight and height from a recent visit.
Qualifying conditions with specific criteria: While a prescriber might accept your report of high blood pressure, insurance may require documented blood pressure readings above certain thresholds, or evidence of treatment with specific medications.
Step therapy requirements: Some plans require you to try older, cheaper weight loss medications (like phentermine or orlistat) before approving GLP-1 medications. You may need to demonstrate that these alternatives didn’t work or weren’t tolerated.
Ongoing authorization: Coverage may be contingent on demonstrating continued weight loss. If you don’t lose a certain percentage of body weight within a specified timeframe, coverage might be discontinued.
For a complete walkthrough of the insurance process, see our Ozempic insurance coverage guide.
Cash-Pay Eligibility
When you’re paying out of pocket, insurance requirements become irrelevant. The only eligibility that matters is what the prescribing provider determines is medically appropriate.
Cash-pay patients generally face more straightforward eligibility assessment. If you meet standard BMI criteria (30+ or 27+ with qualifying conditions) and don’t have contraindications, most providers will prescribe. There’s no insurance company adding additional hurdles.
This doesn’t mean cash-pay is a way to get medication you don’t qualify for. Responsible providers still apply clinical criteria and won’t prescribe for patients who aren’t appropriate candidates. But the process is typically faster and involves fewer bureaucratic obstacles.
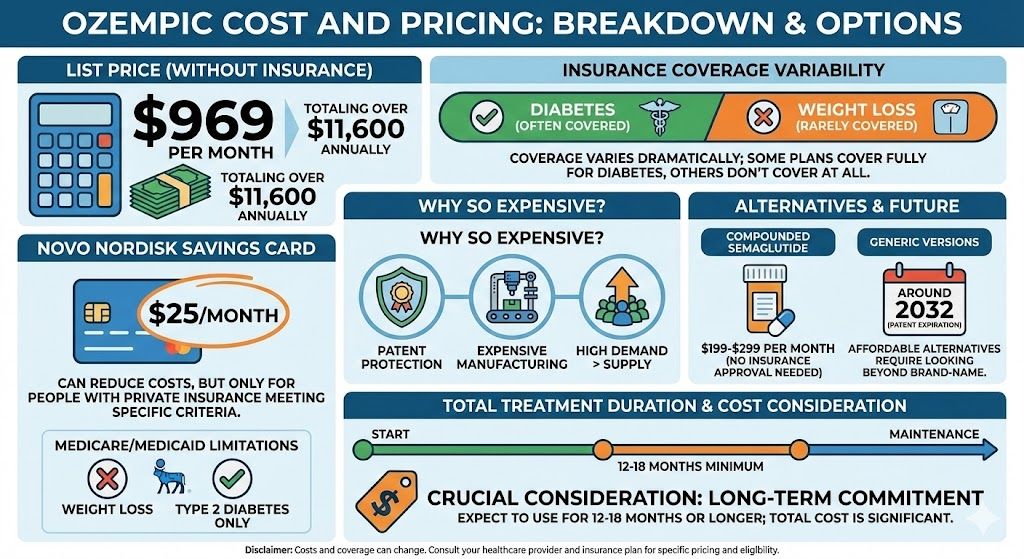
Cash-pay costs have become more accessible in recent months. Brand-name semaglutide (Ozempic or Wegovy) is available at $349/month through Novo Nordisk’s NovoCare program, with introductory pricing of $199 for the first two months. Compounded semaglutide through TrimRx costs $199/month ongoing, making long-term treatment more affordable.
What If You’re Below the BMI Threshold?
Not everyone who wants semaglutide meets the standard eligibility criteria. Here’s what to know if you’re below the thresholds.
BMI 27-29.9 Without Documented Conditions
If your BMI falls in the 27-30 range but you don’t have documented weight-related health conditions, your first step should be getting evaluated for conditions you might not know you have.
Request comprehensive bloodwork including fasting glucose, HbA1c, lipid panel, and liver enzymes. Have your blood pressure checked accurately (not just a quick reading, but proper technique with appropriate rest beforehand). Discuss any symptoms that might indicate sleep apnea, joint problems, or other weight-related issues.
Many people in this BMI range have undiagnosed prediabetes, borderline hypertension, or elevated cholesterol. Identifying these conditions serves two purposes: it establishes eligibility for treatment, and it reveals health issues you should know about regardless of medication decisions.
If comprehensive evaluation reveals no qualifying conditions, you’re in a gray area. Some providers may still prescribe if they believe you’d benefit, particularly if your weight is trending upward or you have other compelling factors. Others will decline to prescribe without qualifying conditions. Telehealth and second opinions may yield different results.
BMI Below 27
If your BMI is below 27, getting semaglutide for weight loss becomes genuinely difficult, and there are good reasons for this.
The medication was studied and approved for people with significant excess weight. Below BMI 27, you’re in the “overweight” or “normal” category where the health impacts of excess weight are less clear and the benefit-risk calculation for medication is less favorable. Semaglutide has real side effects and costs, and prescribing it for people without meaningful medical need isn’t appropriate.
That said, there are edge cases. If you have Type 2 diabetes, Ozempic can be prescribed for blood sugar control regardless of BMI, and weight loss happens as a side effect. If you’re an athlete with high muscle mass and your BMI doesn’t reflect your actual body fat, some providers might consider this. But these are exceptions, not the norm.
For people below BMI 27 without diabetes, the honest answer is that semaglutide probably isn’t appropriate for you right now. Focus on lifestyle approaches to weight management. If your weight increases to the point of meeting criteria, or if you develop qualifying health conditions, medication becomes an option.
The Ethics of Eligibility Thresholds
Some patients feel frustrated by BMI cutoffs, viewing them as arbitrary barriers to treatment they want. It’s worth understanding why these thresholds exist and why prescribers take them seriously.
Medications have risks. Semaglutide can cause gastrointestinal side effects, and rare but serious risks include thyroid tumors (in animal studies), pancreatitis, and gallbladder problems. For patients with significant obesity, these risks are clearly outweighed by the health benefits of substantial weight loss. For patients who are mildly overweight, the calculation is less clear.
Prescribing medication for patients who don’t meet established criteria also exposes providers to professional and legal risk. If a patient experiences a serious adverse event while taking a medication they didn’t qualify for, the prescriber’s decision-making comes under scrutiny.
Finally, there are broader societal considerations. GLP-1 medications have faced supply constraints, and inappropriate prescribing for patients who don’t need them can limit access for patients who do. This isn’t about gatekeeping; it’s about ensuring medications are used for their intended purpose.
Special Situations and Edge Cases
Several common scenarios don’t fit neatly into standard eligibility frameworks. Here’s how they’re typically handled.
Athletes and Muscular Individuals
BMI famously misclassifies some athletes and highly muscular individuals as overweight or obese when they have low body fat. If you’re genuinely in this category (serious athletes, not casual gym-goers), BMI may not accurately reflect your health status.
Providers who recognize this limitation may consider body composition testing (like DEXA scans) or waist circumference measurements as additional data points. Waist circumference above 40 inches for men or 35 inches for women is associated with increased health risk regardless of BMI.
However, be honest with yourself here. The number of people whose BMI is falsely elevated due to muscle mass is much smaller than the number who believe this applies to them. If you’re not consistently training at a high level, standard BMI thresholds probably apply to you.
Recent Weight Gain or Loss
If you’ve recently gained weight and now meet BMI thresholds, you qualify. There’s no requirement for how long you’ve been at a particular weight. That said, providers may want to understand the circumstances of recent weight gain to ensure medication is appropriate.
If you’ve recently lost weight through other means and now fall below thresholds, most providers won’t prescribe. The thresholds apply to your current weight, not your historical maximum. However, if you’re using semaglutide for weight maintenance after significant loss, continuing treatment is often appropriate even if your BMI has dropped below 30.
Pregnancy Planning
Semaglutide is contraindicated during pregnancy and should be stopped at least two months before attempting to conceive. This creates a timing issue for women of childbearing age who want to lose weight before pregnancy.
If you’re planning to become pregnant in the near future, discuss this timeline with your provider. Some may be reluctant to start medication that will need to be stopped soon. Others recognize that losing weight before pregnancy can improve outcomes and will prescribe with clear understanding of the timeline.
Age Considerations
Semaglutide is approved for adults. For adolescents (ages 12+), Wegovy has specific approval with different considerations. Standard adult BMI cutoffs don’t apply the same way to adolescents, and prescribing requires specialized evaluation.
For older adults, standard BMI thresholds apply, but providers may consider additional factors like frailty, nutritional status, and medication interactions. Weight loss in elderly patients carries different considerations than in younger adults.
Post-Bariatric Surgery Patients
Patients who have had bariatric surgery (gastric bypass, sleeve gastrectomy, etc.) and either regained weight or haven’t lost enough weight sometimes seek semaglutide as an additional tool. This can be appropriate but requires careful evaluation.
Post-surgical anatomy may affect how oral medications are absorbed. Semaglutide is injected rather than oral, which bypasses this concern, but the combination of bariatric surgery and GLP-1 medication still requires specialized oversight. If you’re in this situation, work with providers experienced in both bariatric and medical weight management.
How to Prepare for Your Eligibility Evaluation
Regardless of where you seek treatment, coming prepared improves your experience and helps ensure accurate assessment.
Know Your Numbers
Before your appointment or consultation, gather your current weight (ideally from a recent accurate measurement), height, and calculate your BMI. If you have recent bloodwork, know your fasting glucose, HbA1c, and cholesterol numbers. Know your typical blood pressure readings.
Having this information ready demonstrates that you’ve thought seriously about treatment and helps move the conversation forward efficiently.
Document Your Health Conditions
Make a list of any diagnosed conditions that might be weight-related: diabetes, prediabetes, hypertension, high cholesterol, sleep apnea, fatty liver disease, PCOS, joint problems, etc. Include when each was diagnosed, how it’s being treated, and whether it’s currently controlled.
If you suspect you have conditions that haven’t been formally diagnosed, note those as well. Mentioning that you snore heavily and wake up tired (possible sleep apnea) or that your blood pressure readings have been creeping up (possible hypertension) gives your provider information to investigate.
Bring Medical Records If Possible
If you’re seeing a new provider or using telehealth, relevant medical records help verify your health history. This might include recent lab results, a problem list from your primary care doctor, or documentation of specific conditions.
Records aren’t always required, but they strengthen your case if you’re in a borderline eligibility situation and help ensure nothing important is missed.
Be Honest About Your Weight History
Prepare to discuss your weight over time, including your highest adult weight, weight fluctuations, and previous weight loss attempts. This information helps providers understand your situation and assess whether medication is appropriate.
Don’t inflate or minimize your history. If you’ve never seriously committed to lifestyle changes, admit that. If you’ve tried multiple programs without lasting success, explain what happened. Honesty leads to better care.
For comprehensive guidance on navigating the prescription conversation, see our guide on how to ask your doctor for Ozempic.
Frequently Asked Questions
What BMI do I need to get Ozempic?
The standard eligibility threshold for semaglutide treatment for weight loss is a BMI of 30 or higher, which meets the clinical definition of obesity. If your BMI falls between 27 and 29.9, you can still qualify if you have at least one weight-related health condition such as Type 2 diabetes, prediabetes, hypertension, high cholesterol, or sleep apnea. Below BMI 27, most providers won’t prescribe semaglutide for weight loss, though there are exceptions for patients who have Type 2 diabetes (where Ozempic is prescribed for blood sugar control rather than weight). These thresholds come from the FDA approval criteria for Wegovy and have become the standard for prescribing semaglutide for weight management.
Can I get Ozempic if my BMI is 28?
Yes, you can qualify for semaglutide at BMI 28 if you have at least one weight-related health condition. Qualifying conditions include Type 2 diabetes, prediabetes, hypertension (high blood pressure), dyslipidemia (high cholesterol or triglycerides), obstructive sleep apnea, cardiovascular disease, fatty liver disease, and certain other weight-related conditions. The condition needs to be documented in your medical records, either through a formal diagnosis, lab results meeting diagnostic criteria, or evidence of treatment. If you’re at BMI 28 without any documented conditions, ask your doctor to run comprehensive bloodwork and assessments. You may have undiagnosed prediabetes, elevated cholesterol, or other qualifying conditions.
Why is there a BMI requirement for weight loss medication?
BMI requirements exist because medications have both benefits and risks, and the thresholds help identify patients for whom benefits clearly outweigh risks. At BMI 30 and above, excess weight significantly increases the risk of serious health conditions including Type 2 diabetes, cardiovascular disease, certain cancers, and early death. The health benefits of substantial weight loss in this population clearly justify the costs and potential side effects of medication. Between BMI 27 and 30, the picture is more mixed, which is why additional qualifying conditions are required to demonstrate that excess weight is actively harming health. Below BMI 27, the health impacts of excess weight are less clear, and the benefit-risk balance doesn’t favor pharmacological treatment.
Is the BMI requirement different for Ozempic versus Wegovy?
The practical eligibility requirements are similar, but the technical details differ. Ozempic is FDA-approved for Type 2 diabetes, not weight loss, so it technically has no BMI requirement for its approved use. Any patient with Type 2 diabetes can receive Ozempic regardless of weight. When doctors prescribe Ozempic off-label for weight loss, they typically apply the same BMI 30/27 criteria used for Wegovy. Wegovy is FDA-approved specifically for chronic weight management and carries the explicit eligibility criteria of BMI 30+ or BMI 27+ with a weight-related comorbidity. For most patients seeking semaglutide for weight loss, the eligibility assessment is the same regardless of which brand they ultimately receive.
My BMI is 29 but I feel like I need to lose weight. Can I still qualify?
At BMI 29, you fall in the category where you need a qualifying health condition to be eligible for semaglutide. Your feeling that you need to lose weight may be valid, but prescribers need objective criteria to justify medication with real risks and costs. The first step is to get thoroughly evaluated for conditions you might not realize you have. Request comprehensive bloodwork including fasting glucose, HbA1c, and a lipid panel. Get an accurate blood pressure assessment. Discuss any symptoms that might suggest sleep apnea, joint problems, or other weight-related issues. Many people in your BMI range have undiagnosed prediabetes, borderline hypertension, or elevated cholesterol that would qualify them for treatment.
Does insurance have different BMI requirements than doctors?
Yes, insurance companies often apply stricter eligibility criteria than medical prescribing standards. While a doctor might prescribe semaglutide based on meeting basic BMI thresholds, insurance prior authorization typically requires additional documentation. This might include evidence of previous weight loss attempts, specific documentation of BMI from a clinical visit, proof of qualifying conditions meeting certain criteria, and sometimes completion of step therapy (trying older medications first). Insurance requirements vary significantly by plan, and some plans don’t cover weight loss medications at all. Cash-pay options avoid these additional hurdles, with eligibility determined solely by medical appropriateness as assessed by the prescribing provider.
How is BMI calculated and why do some people say it’s inaccurate?
BMI is calculated by dividing weight in kilograms by height in meters squared (or weight in pounds divided by height in inches squared, multiplied by 703). It’s a simple ratio that provides a rough estimate of body fatness at the population level. Critics correctly point out that BMI doesn’t distinguish between muscle and fat, meaning some muscular individuals are classified as overweight despite low body fat. BMI also doesn’t account for fat distribution, which affects health risk. Additionally, the standard thresholds were developed primarily using white European populations and may not be equally applicable across all ethnicities. Despite these limitations, BMI remains the standard clinical screening tool because it’s simple, inexpensive, and correlates reasonably well with health outcomes for most people.
Can waist circumference qualify me instead of BMI?
Waist circumference is recognized as a meaningful health metric and is sometimes used alongside BMI in clinical assessments, but it typically doesn’t replace BMI for determining semaglutide eligibility. The FDA approval criteria for Wegovy specify BMI thresholds, so that’s what prescribers generally use. However, some providers may consider waist circumference as supporting evidence, particularly in borderline cases. Waist circumference above 40 inches for men or 35 inches for women is associated with increased health risk and may indicate metabolic dysfunction even at lower BMI levels. If your BMI is borderline and your waist circumference is elevated, mentioning this to your provider could support your case.
What if my doctor won’t prescribe because of BMI requirements?
If your doctor declines to prescribe and you believe you meet eligibility criteria, you have several options. First, clarify why they’re declining. Is it truly about BMI, or are there other concerns? If you’re close to thresholds, ask about getting evaluated for qualifying conditions you might not know you have. If your doctor simply doesn’t prescribe these medications, ask for a referral to an endocrinologist or obesity medicine specialist. You can also explore telehealth platforms like TrimRx that specialize in weight management and evaluate patients specifically for GLP-1 eligibility. A “no” from one provider doesn’t mean you won’t qualify elsewhere, but if multiple providers are declining, consider whether the eligibility concerns are legitimate.
If I lose weight on Ozempic and my BMI drops below 30, will I lose my prescription?
Generally, no. Once you’ve started treatment and are losing weight successfully, most providers will continue prescribing even if your BMI drops below the initial threshold. The goal is sustained weight loss and improved health, not reaching a BMI number and stopping. In fact, clinical evidence shows that patients who stop semaglutide typically regain a significant portion of lost weight, which is why ongoing treatment is often recommended. Insurance is the potential complication here. Some plans require continued eligibility verification and might discontinue coverage if your BMI falls below their thresholds. However, if you’re paying cash and your provider supports continued treatment, your lowered BMI won’t disqualify you from ongoing prescriptions.
Are BMI requirements different for compounded semaglutide?
The eligibility criteria for compounded semaglutide are essentially the same as for brand-name medications. Responsible telehealth platforms and compounding pharmacy partners follow standard medical criteria (BMI 30+ or BMI 27+ with qualifying conditions) because these thresholds reflect appropriate prescribing regardless of the medication source. Compounded semaglutide contains the same active ingredient and works the same way, so there’s no medical reason eligibility would differ. What does differ is the process. Telehealth platforms may be more streamlined in their evaluation, without the multiple appointments and extensive documentation sometimes required by traditional healthcare or insurance. But this efficiency doesn’t mean lower standards. It means focused evaluation specifically for GLP-1 eligibility.
Your Next Steps
Understanding BMI requirements is the first step in determining whether you’re a candidate for semaglutide treatment. If you meet the criteria (BMI 30+ or BMI 27+ with qualifying conditions) and don’t have contraindications, you’re likely eligible for treatment through various pathways.
For many patients, telehealth offers the most accessible route to evaluation and treatment. TrimRx provides consultations with licensed healthcare providers who specialize in weight management and can assess your eligibility based on your individual health profile.
Ready to find out if you qualify? Start your consultation with TrimRx and explore compounded semaglutide at $199/month.

Transforming Lives, One Step at a Time
Keep reading
Ozempic Before and After: Real Results and Timelines
The transformation photos are everywhere. Social media feeds, news articles, celebrity coverage. People showing dramatic weight loss, completely changed body shapes, faces you almost…
How Much Weight Can You Lose on Ozempic? Real Data and Expectations
It’s the first question everyone asks: How much weight will I actually lose? You’ve seen the dramatic before-and-after photos. You’ve heard stories of people…
Ozempic Weight Loss Results: What to Expect Month by Month
You’re considering Ozempic or you’ve just started, and you want to know what’s realistic. How much weight will you actually lose? When will you…



