Semaglutide Side Effects: Complete Guide and Management Tips

Starting semaglutide often comes with a mix of excitement about potential weight loss and anxiety about side effects you’ve heard about. Maybe you’ve read horror stories online about people vomiting for weeks, or maybe your doctor briefly mentioned nausea but didn’t explain what to actually expect.
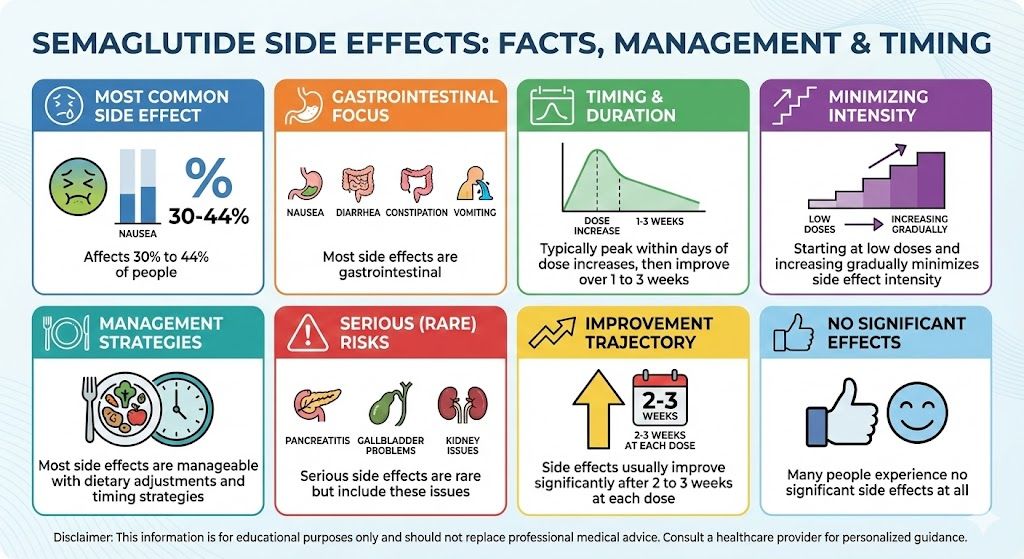
Here’s the reality: most people experience some side effects with semaglutide, particularly during the first few weeks and when doses increase. Nausea tops the list, affecting somewhere between 30% and 44% of people depending on the dose. Digestive issues like diarrhea, constipation, and abdominal discomfort are common. However, these effects are usually manageable with the right strategies, and they typically improve significantly after the first few weeks at each new dose level.
This guide walks through every side effect worth knowing about, from the mild and common to the rare but serious. You’ll learn what to expect, when side effects typically occur, how to minimize them, and when you should contact your healthcare provider.
Key Takeaways: Semaglutide Side Effects
- Nausea is the most common side effect, affecting 30% to 44% of people
- Most side effects are gastrointestinal: nausea, diarrhea, constipation, vomiting
- Side effects typically peak within days of dose increases, then improve over 1 to 3 weeks
- Starting at low doses and increasing gradually minimizes side effect intensity
- Most side effects are manageable with dietary adjustments and timing strategies
- Serious side effects are rare but include pancreatitis, gallbladder problems, and kidney issues
- Side effects usually improve significantly after 2 to 3 weeks at each dose
- Many people experience no significant side effects at all
Most Common Side Effects and Their Frequency
Understanding what you’re likely to encounter helps you prepare and recognize that your experience is normal.
Nausea
Nausea ranks as the single most common side effect across all semaglutide clinical trials. In the STEP-1 trial studying Wegovy at 2.4 mg weekly, about 44% of participants reported nausea at some point during treatment. At lower doses like 0.5 mg or 1 mg, the percentage drops to around 20% to 30%.
The nausea typically follows a predictable pattern. It’s usually worst within the first day or two after your weekly injection, then gradually improves over the next few days. By day five or six after your injection, most people feel close to normal, then the cycle repeats with the next dose.
For many people, the nausea is mild enough to push through without significantly impacting daily activities. You feel slightly queasy, particularly in the morning or after eating, but you can still function. For others, the nausea is more intense during those first few post-injection days, sometimes requiring rest or limiting activities.
The good news is that nausea usually improves substantially after you’ve been at a specific dose for 2 to 3 weeks. Your body adapts. The nausea that felt overwhelming after your first injection at a new dose often becomes much more manageable by your third or fourth injection at that same level.
Diarrhea
About 30% of people experience diarrhea on semaglutide. Like nausea, it tends to be worse during the first few weeks at each new dose and often improves with time.
The diarrhea ranges from mild (slightly looser stools than usual) to more disruptive (multiple urgent bowel movements daily). For most people, it falls somewhere in the middle. You might have one or two episodes of loose stools daily during the adjustment period.
Interestingly, the mechanism behind semaglutide-related diarrhea isn’t entirely clear. It might relate to how the medication affects gut motility and water absorption in your intestines. The slowed gastric emptying can also change the timing and consistency of bowel movements.
Constipation
Paradoxically, constipation is nearly as common as diarrhea, affecting about 24% to 28% of people. Some people even experience alternating episodes of both.
The constipation makes more intuitive sense given how semaglutide works. When your stomach empties more slowly and you’re eating significantly less food, your bowel movements naturally decrease in frequency. Less food going in means less waste coming out.
The reduced food intake also means less fiber consumption if you’re not consciously compensating. Many people naturally gravitate toward simpler, easier-to-digest foods when nauseated, which often means fewer vegetables and whole grains that support regular bowel movements.
Vomiting
Vomiting is less common than nausea but still affects roughly 9% to 15% of people depending on the dose. It usually only happens when nausea is particularly intense, often if you try to eat normal portion sizes despite feeling full.
Most people who experience vomiting find it’s occasional rather than frequent. You might vomit once or twice during the first week at a new dose, then not again. It’s rarely the persistent, severe vomiting that requires medical intervention, though that can happen in rare cases.
Abdominal Pain and Discomfort
About 20% to 25% of people report abdominal discomfort, cramping, or pain. This can range from mild bloating and fullness to sharper cramping sensations, particularly after eating.
The discomfort often relates to the slowed gastric emptying. Your stomach feels uncomfortably full because food is sitting there longer than usual. Sometimes the discomfort comes from eating too much for what your system can handle on the medication.
Decreased Appetite
This is technically the intended effect rather than a side effect, but many people find that the appetite suppression feels almost too extreme, particularly at higher doses. You might have to consciously remind yourself to eat because you simply don’t feel hungry, even when it’s been many hours since your last meal.
Some people describe it as food becoming uninteresting or unappealing. Things you used to crave intensely lose their appeal. The constant mental preoccupation with food that characterized your pre-treatment life simply disappears.
While this is the desired therapeutic effect, it can feel strange and occasionally concerning when you’re not naturally motivated to eat adequate nutrition.
Fatigue
Between 10% and 15% of people report increased fatigue, particularly during the first few weeks at new doses. This likely relates to your body adjusting to significantly reduced calorie intake.
When you suddenly drop from consuming 2,500 calories daily to 1,200 calories, your energy levels can dip until your body adapts. The fatigue usually improves within a few weeks as your metabolism adjusts.
Other Common Effects
Headaches affect about 10% of people, typically during adjustment periods. Dizziness or lightheadedness occurs in roughly 8% to 10%, often related to reduced food intake, dehydration, or blood pressure changes from weight loss. Acid reflux or heartburn worsens for some people due to delayed gastric emptying. Injection site reactions like redness, itching, or small lumps occur occasionally, usually resolved by rotating injection sites.
These effects are generally mild and temporary for most people experiencing them.
Timeline: When Side Effects Occur
Understanding when to expect side effects helps you plan and recognize normal patterns versus concerning developments.
First Injection at Starting Dose
Your very first injection at 0.25 mg usually produces noticeable but manageable side effects. Mild nausea beginning within 24 to 48 hours is common. Some appetite reduction might occur immediately or within a few days. Slight digestive changes including changes in bowel movement frequency or consistency can start within the first few days. Energy levels might dip slightly as your body encounters the medication.
Most people get through their first week without major issues. The starting dose is intentionally low to ease you into treatment.
Weeks 2 Through 4 at Starting Dose
By your second injection at the same 0.25 mg dose, side effects often diminish noticeably. Your body is adapting. Nausea typically improves significantly, becoming milder or less frequent. Digestive issues start normalizing. Energy levels return closer to baseline. Appetite suppression becomes more consistent and less dramatic.
By week four at the starting dose, many people feel they’ve mostly adjusted and side effects are minimal.
First Dose Increase
When you increase from 0.25 mg to 0.5 mg, expect that familiar pattern to repeat. The first injection at the new dose often brings a temporary return of side effects. Nausea usually comes back for a few days, though you might handle it better with experience. Digestive upset might resurface. You might feel more tired for a few days.
This pattern repeats with each dose increase throughout treatment. The first week or two at each new level brings renewed side effects, then improvement as you adapt.
Ongoing Treatment at Stable Doses
Once you’ve been at a specific dose for several weeks and that dose isn’t increasing, side effects typically settle at a low level or disappear entirely. Many people at stable maintenance doses report minimal or no side effects after the initial adjustment period.
However, some people continue experiencing mild intermittent nausea or digestive issues even after months of treatment at the same dose. This is less common but not abnormal.
For detailed information about the full dosing journey, see our complete semaglutide dosage guide.
Managing Nausea: Practical Strategies That Work
Since nausea bothers more people than any other side effect, having effective management strategies makes a huge difference.
Eat Smaller, More Frequent Meals
This advice sounds simple but genuinely helps. Instead of three large meals daily, aim for five or six smaller eating occasions. Your stomach empties slowly on semaglutide, so large meals sit there causing discomfort and nausea for hours.
A small breakfast at 7 AM, a snack at 10 AM, lunch at 1 PM, another snack at 4 PM, and dinner at 7 PM works better than big meals at 8 AM, noon, and 6 PM. Each eating occasion should involve modest portions that leave you satisfied but not overly full.
Focus on Bland, Easy-to-Digest Foods
When nausea is active, particularly in those first few days after injections, stick with gentle foods. Crackers, toast, rice, bananas, applesauce, plain chicken breast, baked potatoes without toppings, and broth-based soups tend to sit well.
Save the rich, fatty, spicy, or heavily seasoned foods for days when you’re feeling better. Those foods aren’t forbidden, but they tend to worsen nausea when your stomach is already sensitive.
Stay Hydrated
Dehydration worsens nausea significantly. Sip water, herbal tea, or clear broths throughout the day. Room temperature or slightly warm fluids often sit better than very cold ones when you’re nauseated.
Aim for at least 64 ounces of fluid daily, more if you’re experiencing vomiting or diarrhea. Small, frequent sips work better than trying to drink large amounts at once.
Try Ginger
Ginger has legitimate anti-nausea properties. Ginger tea, ginger candies, ginger chews, or ginger supplements can provide relief. Some people keep ginger candies with them and suck on one when nausea strikes.
Fresh ginger grated into hot water as tea works well. Crystallized ginger pieces offer a convenient option. Even ginger ale (preferably with real ginger) helps some people, though watch the sugar content.
Avoid Lying Down After Eating
Lying down within an hour or two of eating can worsen nausea and trigger acid reflux. The delayed gastric emptying means food sits in your stomach longer, and lying flat can allow acid and partially digested food to move back toward your esophagus.
Stay upright for at least two hours after eating if possible. If you must lie down, prop yourself up with pillows to maintain some elevation.
Time Your Injection Strategically
Many people find that taking their injection in the evening after dinner helps. The peak nausea period occurs while you’re sleeping or during the next morning when you can take it easy. By afternoon, the worst has passed.
Experiment with timing to find what works for your schedule and symptom pattern.
Consider Anti-Nausea Medications
If nausea remains severe despite dietary strategies, ask your provider about anti-nausea medications. Options like ondansetron (Zofran), metoclopramide, or promethazine can provide relief during the worst periods.
Some people use these medications just for the first few days at each new dose level to get through the adjustment period more comfortably.
Don’t Force Yourself to Eat
When you feel nauseated, eating often feels like the last thing you want to do. Listen to your body. If you’re not hungry and feeling queasy, it’s okay to skip a meal or just have something very light.
Forcing yourself to eat normal portions when nauseated often leads to vomiting and makes the nausea worse. Eat what you can comfortably handle and don’t stress about meeting specific calorie targets during the worst nausea days.
Managing Digestive Issues: Diarrhea and Constipation
The other major category of side effects involves bowel function changes. Strategies differ depending on which direction things go.
For Diarrhea
Stay very well hydrated to replace fluid losses. Water, clear broths, diluted sports drinks, and oral rehydration solutions help maintain electrolyte balance. Stick to bland, low-fiber foods during active diarrhea episodes. White rice, bananas, toast, and plain crackers are gentle options. Avoid caffeine, alcohol, fatty foods, and dairy products (unless you normally tolerate dairy well), as these can worsen diarrhea.
Consider a probiotic supplement to support gut health. Some evidence suggests probiotics help regulate bowel function during GLP-1 medication use. Over-the-counter anti-diarrheal medications like loperamide can provide temporary relief if diarrhea is disruptive, though check with your provider before regular use.
If diarrhea persists beyond 2 to 3 weeks at a stable dose or becomes severe enough to cause dehydration, contact your provider.
For Constipation
Increase fluid intake substantially. Many people don’t realize that mild dehydration contributes significantly to constipation. Aim for 80 to 100 ounces of water daily when constipated. Add fiber gradually through vegetables, fruits, whole grains, or psyllium supplements. However, add fiber slowly because too much too fast can worsen bloating and discomfort.
Stay physically active. Movement helps stimulate bowel function. Even gentle walking for 20 to 30 minutes daily helps. Consider a gentle stool softener like docusate sodium (Colace). These help keep stools soft without causing cramping or urgency.
For more stubborn constipation, osmotic laxatives like polyethylene glycol (Miralax) are generally safe for regular use. They draw water into your colon to soften stools. Avoid stimulant laxatives (like senna or bisacodyl) for regular use, as these can create dependency.
Ensure you’re eating adequate food despite reduced appetite. Very low food intake inevitably means less frequent bowel movements. Some reduction in frequency is normal and not necessarily problematic unless you’re experiencing discomfort.
For Alternating Issues
Some people experience both diarrhea and constipation at different times. This can be particularly frustrating. Focus on consistent hydration, balanced fiber intake, and regular eating patterns to help regulate function. Keep both stool softeners and anti-diarrheal medication on hand to use as needed.
If the alternating pattern persists or worsens, discuss with your provider whether staying at your current dose longer before increasing might help your digestive system adapt more fully.
Serious Side Effects: When to Seek Medical Attention
While most side effects are uncomfortable but not dangerous, certain symptoms require prompt medical evaluation.
Pancreatitis
Pancreatitis is inflammation of the pancreas. It’s rare but can be serious. Warning signs include severe abdominal pain, often in the upper abdomen radiating to your back. The pain is persistent, intense, and doesn’t improve with position changes or over-the-counter pain relievers. Nausea and vomiting accompanying the severe pain, fever, and rapid pulse can occur.
If you experience severe, persistent abdominal pain, stop taking semaglutide and contact your healthcare provider or go to an emergency room immediately.
Risk factors for pancreatitis on GLP-1 medications include history of pancreatitis, gallstones, high triglycerides, and heavy alcohol use.
Gallbladder Problems
Rapid weight loss increases the risk of gallstones, which can lead to gallbladder inflammation (cholecystitis). Symptoms include pain in your upper right abdomen, often after eating fatty meals. Pain that radiates to your right shoulder blade, nausea and vomiting, and fever can accompany gallbladder issues.
If you develop these symptoms, contact your provider. Many gallbladder issues require medical evaluation and sometimes surgery.
Kidney Problems
Kidney issues on semaglutide usually relate to severe dehydration from persistent vomiting or diarrhea rather than direct kidney toxicity. Warning signs include decreased urination or very dark urine, swelling in your legs, ankles, or feet, significant fatigue and confusion, and persistent nausea.
If you notice these symptoms, particularly if you’ve been vomiting or having diarrhea, seek medical attention.
Severe Allergic Reactions
Though rare, allergic reactions can occur. Seek immediate medical help if you experience difficulty breathing or swallowing, severe rash or hives over large areas of your body, swelling of your face, lips, tongue, or throat, rapid heartbeat, or dizziness and fainting.
Vision Changes
Some people with diabetes have reported worsening diabetic retinopathy when starting GLP-1 medications, possibly related to rapid blood sugar improvement. If you notice sudden vision changes, blurriness that doesn’t resolve, or dark spots in your vision, contact your eye doctor and diabetes care provider.
Thyroid Concerns
Semaglutide carries a boxed warning about thyroid C-cell tumors based on animal studies. This hasn’t been confirmed in humans, but don’t use semaglutide if you have a personal or family history of medullary thyroid cancer or Multiple Endocrine Neoplasia syndrome type 2.
If you develop a lump in your neck, hoarseness that doesn’t resolve, trouble swallowing, or shortness of breath, get evaluated promptly.
Side Effects at Different Dose Levels
Side effect frequency and intensity vary across the dosing schedule.
At 0.25 mg weekly, most people experience mild effects. Nausea occurs but is usually manageable. Digestive changes are noticeable but not typically disruptive. This starting dose is designed to minimize side effects while introducing the medication.
At 0.5 mg weekly, side effects increase in frequency and intensity for many people. Nausea becomes more pronounced, especially during the first week at this dose. Appetite suppression strengthens noticeably. Digestive issues may intensify temporarily.
At 1 mg weekly, this dose often represents a threshold where semaglutide’s effects become quite powerful. Side effects during the first week at 1 mg can be challenging for some people. However, after 2 to 3 weeks at this dose, many people feel well-adjusted.
At 1.7 mg weekly, expect another bump in side effects when first increasing to this level. The jump from 1 mg to 1.7 mg is substantial. Nausea often returns even if it had mostly resolved at 1 mg. Appetite suppression can feel almost too extreme.
At 2.4 mg weekly (maximum dose), the final increase to 2.4 mg can bring another wave of side effects. Not everyone needs this highest dose, and some people choose to stay at 1.7 mg if they’re getting good results with manageable side effects.
For comprehensive information about the complete dosing schedule and what to expect at each level, see our semaglutide weight loss results guide.
Long-Term Side Effects and Considerations
Most discussion focuses on initial side effects, but what about long-term use?
After several months at a stable dose, most people find side effects are minimal or absent. Your body has fully adapted. However, some people continue experiencing mild intermittent nausea, particularly if they eat too much at once or consume rich foods. Occasional digestive irregularities persist for some. Reduced appetite continues, which is the intended effect.
One concern with long-term GLP-1 medication use is potential muscle loss alongside fat loss. When you lose weight rapidly while eating significantly less, some muscle loss typically occurs along with fat loss. Prioritizing protein intake and incorporating resistance training helps preserve muscle mass.
Some people report hair thinning several months into treatment. This usually relates to rapid weight loss and reduced calorie/nutrient intake rather than direct medication effects. It typically resolves once weight stabilizes.
Bone health is an area of ongoing research. Rapid weight loss can affect bone density. Ensuring adequate calcium, vitamin D, and weight-bearing exercise supports bone health during treatment.
The medication doesn’t appear to lose effectiveness over time (tolerance doesn’t develop), which is good news for long-term weight maintenance. People who stay on semaglutide can maintain their weight loss as long as they continue treatment.
Comparing Semaglutide Side Effects to Other Medications
Understanding how semaglutide’s side effect profile compares to alternatives provides useful context.
Semaglutide versus tirzepatide shows similar side effects overall, though tirzepatide causes gastrointestinal issues slightly more frequently. Nausea, diarrhea, and digestive discomfort occur in about 5% to 10% more people on tirzepatide. This likely relates to tirzepatide’s dual GIP and GLP-1 action creating stronger gut effects.
For detailed comparison, see our Mounjaro vs Ozempic guide.
Semaglutide versus liraglutide presents fewer side effects than liraglutide in many people’s experience. Liraglutide requires daily injections and has a shorter half-life, creating more frequent peaks and troughs that can mean more variable side effects throughout each day.
Semaglutide versus older weight loss medications like phentermine causes different side effect types. Phentermine can cause jitteriness, increased heart rate, difficulty sleeping, and elevated blood pressure. Semaglutide’s side effects are primarily digestive. Neither profile is objectively better, just different.
Compared to bariatric surgery, semaglutide offers similar weight loss results for many people without surgical risks, recovery time, or permanent anatomical changes. However, surgery comes with its own side effect profile including surgical complications, dumping syndrome, nutritional deficiencies, and need for vitamin supplementation.
Minimizing Side Effects: Prevention Strategies
While you can’t completely avoid side effects, certain approaches minimize their intensity.
Follow the titration schedule carefully. Never skip the gradual dose escalation even if you’re tolerating lower doses easily. The standard schedule exists specifically to minimize side effects. Start with the lowest 0.25 mg dose and increase only every four weeks minimum.
Stay well hydrated from day one. Don’t wait until you’re experiencing side effects to focus on hydration. Adequate fluid intake from the beginning helps with nausea, constipation, and overall medication tolerance.
Adjust your eating immediately. Don’t wait until nausea forces smaller portions. Start eating smaller, more frequent meals from your very first injection. This proactive approach prevents the worst side effects rather than reacting to them.
Choose bland, gentle foods during the first few days after each injection, especially at new dose levels. You can gradually reintroduce richer foods as you adjust.
Time your injections thoughtfully. If evening injections allow you to sleep through peak nausea, do that. If morning injections work better for your schedule and symptom pattern, that’s fine too.
Rotate injection sites consistently to prevent injection site reactions. Use your abdomen one week, thighs the next, upper arms after that, then back to abdomen.
Stay physically active. Regular movement helps with nausea, digestive function, energy levels, and overall wellbeing. Even gentle walking helps.
Communicate with your provider. If side effects are problematic, your provider can suggest staying at your current dose longer, temporarily reducing your dose, or implementing other management strategies. Don’t suffer in silence.
When Side Effects Mean You Should Stop
Most side effects are manageable, but certain situations warrant discontinuing semaglutide.
Severe, persistent vomiting that prevents adequate hydration creates a medical emergency. If you can’t keep fluids down for 24 hours or more, seek medical attention and discuss whether continuing treatment makes sense.
Intolerable side effects that significantly impair your quality of life despite management attempts might make treatment unsustainable. If nausea is so severe you can’t work or function, or if side effects are causing significant anxiety or depression, the benefits may not outweigh the costs.
Development of serious complications like pancreatitis means stopping immediately. If confirmed pancreatitis occurs, you shouldn’t restart semaglutide.
Severe allergic reactions require immediate discontinuation and emergency treatment.
Some people simply don’t tolerate semaglutide well despite trying multiple strategies. This doesn’t mean you’re weak or doing something wrong. Individual variation in medication tolerance is normal. Other weight loss approaches might work better for you.
If you need to stop semaglutide, discuss alternative options with your provider. Compounded tirzepatide might be better tolerated by some people who struggle with semaglutide, though it can cause similar side effects. Traditional weight loss approaches combining diet, exercise, and behavioral support remain effective for many people.
For information about what happens after stopping, including how long side effects persist, see our guide to how long semaglutide stays in your system.
Frequently Asked Questions
What are the most common side effects of semaglutide?
The most common side effects are gastrointestinal. Nausea affects 30% to 44% of people, diarrhea occurs in about 30%, constipation affects 24% to 28%, and vomiting happens in 9% to 15%. Abdominal discomfort, reduced appetite, and fatigue are also common. Most of these effects are worst during the first few weeks at each new dose level and typically improve significantly after 2 to 3 weeks of consistent dosing.
How long do semaglutide side effects last?
Most side effects are temporary, lasting 1 to 3 weeks at each new dose level. They typically peak within the first few days after dose increases, then gradually improve as your body adapts. After several weeks at a stable dose, many people experience minimal or no side effects. However, some people continue having mild intermittent nausea or digestive issues even after months of treatment.
Does semaglutide nausea go away?
Yes, nausea usually improves significantly within 2 to 3 weeks at each dose level as your body adjusts. The nausea is typically worst during the first week at a new dose, particularly in the first day or two after your injection. It becomes progressively milder with each subsequent injection at the same dose. Some people continue experiencing mild nausea intermittently, but the severe nausea most people worry about typically resolves with time.
How can I reduce side effects from semaglutide?
Eat smaller, more frequent meals rather than large portions. Stick to bland, easy-to-digest foods, especially in the first few days after injections. Stay very well hydrated throughout each day. Avoid fatty, greasy, or spicy foods when feeling nauseated. Don’t lie down immediately after eating. Try ginger in various forms for nausea relief. Consider timing your injection for evenings so peak side effects occur during sleep. Follow the gradual dose escalation schedule carefully without rushing increases.
Can you take anti-nausea medication with semaglutide?
Yes, anti-nausea medications can be used alongside semaglutide. Options like ondansetron (Zofar), metoclopramide, or promethazine often help manage severe nausea. Discuss with your healthcare provider which anti-nausea medication would be most appropriate for your situation. Some people use these medications just during the first few days at new dose levels to make the adjustment period more tolerable.
What are the serious side effects of semaglutide?
Serious but rare side effects include pancreatitis (severe abdominal pain radiating to the back), gallbladder problems (upper right abdominal pain, especially after eating), kidney problems (usually related to severe dehydration), severe allergic reactions (difficulty breathing, severe rash, facial swelling), and vision changes (particularly in people with diabetes). These require immediate medical attention. The medication also carries a warning about thyroid tumors based on animal studies, though this hasn’t been confirmed in humans.
Why does semaglutide cause nausea?
Semaglutide causes nausea primarily by slowing gastric emptying, meaning food stays in your stomach longer than usual. This creates feelings of fullness that can tip into discomfort and nausea, especially if you eat normal-sized portions. The medication also activates GLP-1 receptors in areas of your brain that control nausea responses. These combined effects make nausea the most common side effect.
Do side effects get worse with higher doses of semaglutide?
Side effects often temporarily worsen when you increase to each new dose level. The jump from one dose to the next brings a return of side effects similar to when you first started, though many people handle subsequent increases better with experience. However, after 2 to 3 weeks at the new dose, side effects typically settle back down to manageable levels or resolve. The highest doses (1.7 mg and 2.4 mg) tend to cause more side effects than lower doses.
Can semaglutide cause long-term side effects?
Most concerning long-term effects relate to rapid weight loss rather than the medication directly. These include potential muscle loss if protein intake is inadequate, possible hair thinning several months into treatment (usually temporary), and bone density changes with rapid weight loss. The medication itself doesn’t cause significant long-term side effects in most people who tolerate it well initially. Ongoing research continues monitoring long-term safety.
What should I do if side effects are unbearable?
Contact your healthcare provider immediately if side effects are severely impacting your quality of life. Options include staying at your current dose longer before increasing, temporarily reducing to your previous dose level, implementing more aggressive side effect management strategies, or in some cases discontinuing treatment. Never suffer through unbearable side effects without discussing alternatives with your provider. Some people do better on different medications like tirzepatide or respond better after adjusting the titration schedule.
Managing Your Semaglutide Journey Successfully
Side effects are a reality for most people taking semaglutide, but they’re usually manageable with the right strategies and realistic expectations. The overwhelming majority of side effects are temporary, improving significantly within weeks as your body adapts to each dose level. Very few people experience the severe, ongoing side effects that dominate online discussion forums.
The key is preparation and proactive management. Start with appropriate expectations about what you’ll likely experience. Implement dietary and lifestyle strategies from day one rather than waiting for problems to develop. Communicate openly with your healthcare provider about what you’re experiencing and what’s working or not working. Be patient with the gradual dose escalation process, even when it feels slow.
Most people who stick with semaglutide through the initial adjustment period achieve significant weight loss results that make the temporary discomfort worthwhile. Understanding that side effects are usually temporary and manageable helps you push through the challenging early weeks to reach the benefits on the other side.
Whether you’re using brand-name semaglutide or more affordable compounded semaglutide at $199 monthly through TrimRx, the side effect profile remains the same because it’s inherent to the medication’s mechanism of action. Get started with comprehensive medical oversight and support throughout your treatment journey, including guidance on managing side effects effectively at every stage.

Transforming Lives, One Step at a Time
Keep reading
GLP-1 Telehealth on the West Coast: CA, WA and OR
The West Coast has a reputation for progressive healthcare policy and high insurance coverage rates, and in many respects that reputation is earned. California,…
GLP-1 Telehealth in the Southwest: TX, AZ, NV and NM
The Southwest is a region of stark contrasts when it comes to healthcare access. Phoenix and Las Vegas are sprawling, fast-growing metros with expanding…
GLP-1 Telehealth in the Midwest: IL, OH, MI and IN
The Midwest doesn’t get as much attention in conversations about obesity and healthcare access as the South does, but the numbers tell a sobering…



