Semaglutide Stopped Working: Next Steps

If semaglutide was producing steady weight loss and then stopped, you’re experiencing a plateau, and it’s one of the most common phases in GLP-1 treatment. Semaglutide hasn’t become ineffective. Your body has adapted to its new, lower weight, and the conditions that were driving your initial results have shifted. The most common causes include metabolic adaptation to weight loss, a dose that no longer matches your needs, gradual dietary drift, loss of lean muscle mass, or an underlying medical factor that’s emerged during treatment. Breaking through requires identifying which of these is at play and making targeted adjustments.
Here’s how to work through it systematically.
What’s Actually Happening When Semaglutide “Stops Working”
Semaglutide doesn’t build tolerance the way some drugs do. It continues to bind to GLP-1 receptors, slow gastric emptying, and influence appetite signaling in the brain at the same dose. What changes is the context around it.
When you lose weight, your body’s calorie needs decrease. A person who has gone from 220 pounds to 190 burns meaningfully fewer calories at rest. Their basal metabolic rate has dropped. Meanwhile, a process called adaptive thermogenesis kicks in, where your body becomes slightly more efficient at using calories, burning fewer than predicted by weight alone. Research published in Obesity (Martins et al., 2020) demonstrated that this metabolic adaptation can reduce daily energy expenditure by 100 to 300 calories beyond what weight loss alone would predict.
So the calorie deficit that produced consistent results at your starting weight may have quietly shrunk to zero at your current weight. You’re eating the same amount, but your body now needs less. The math no longer works, and the scale flatlines.
This is biology, not medication failure.
Step 1: Evaluate Whether You Need a Dose Increase
Semaglutide for weight loss is dosed up to 2.4 mg weekly (Wegovy dosing) or up to 2 mg (Ozempic dosing). If you’re on a lower dose and your progress has stalled, moving up is often the most direct solution.
Each dose increase tends to restore some degree of appetite suppression and metabolic benefit. Many patients who feel like the medication stopped working at 1 mg find that results restart at 1.7 mg or 2.4 mg. The semaglutide timeline shows how weight loss often follows a staircase pattern, with renewed progress after each dose step-up.
If you’re already at the maximum dose, this option is off the table, but there are still plenty of other levers to pull. And if you’ve maxed out on semaglutide entirely, switching to a different medication class is worth discussing (more on that below).
Step 2: Audit Your Actual Food Intake
This step is uncomfortable for most people, but it’s also the most commonly needed one. Dietary drift is real, and it happens gradually enough that you won’t notice it without actively looking.
Here’s what typically happens. During the first few months on semaglutide, appetite suppression is at its strongest. You eat small portions naturally, skip snacks without thinking about it, and feel satisfied easily. Over time, your brain partially adapts to the medication’s signaling. Hunger creeps back in, not to pre-treatment levels, but enough that portions start growing, snacks reappear, and calorie-dense convenience foods show up more often.
Consider this scenario: a patient was eating about 1,200 calories daily during their best weight loss months. Six months later, without deliberately changing anything, they’re averaging 1,600. They don’t feel like they’re eating more. But at their new, lower body weight, 1,600 calories is maintenance, not a deficit.
Track everything for five to seven days. Use a food scale for portions. Include cooking oils, dressings, beverages, and the bites you take while cooking. The data almost always reveals a gap between perception and reality.
Step 3: Protect and Rebuild Muscle Mass
Muscle loss during weight loss is the silent metabolism killer that most people overlook. When you lose weight through calorie restriction alone, roughly 25% to 30% of the weight lost can come from lean mass rather than fat. That’s a significant hit to your resting metabolic rate, since muscle tissue is metabolically active in ways that fat tissue isn’t.
The practical impact: every pound of muscle lost reduces your daily calorie burn by about six calories at rest. Lose 10 pounds of muscle over several months of treatment, and your body now burns 60 fewer calories per day than it would have otherwise. Over a year, that’s equivalent to about six pounds of fat your body would have burned but didn’t.
The solution is resistance training, and it doesn’t have to be extreme. Two to three sessions per week of compound exercises (squats, lunges, rows, presses, deadlifts) provides enough stimulus to preserve existing muscle and potentially regain some of what was lost. Pair this with adequate protein, aiming for at least 0.7 to 1 gram per pound of your current body weight daily.
The semaglutide first week article covers initial body composition changes, but muscle preservation becomes even more important the further you get into treatment.
Step 4: Increase Your Daily Movement
Formal exercise gets most of the attention, but your non-exercise movement throughout the day (called NEAT, or non-exercise activity thermogenesis) often has a bigger impact on total calorie burn. NEAT includes walking, standing, cleaning, fidgeting, taking stairs, and all the small movements you do without thinking about them.
Here’s the catch: when you’re in a calorie deficit, your body unconsciously reduces NEAT. You sit more. You move slower. You choose the elevator. You rest between tasks instead of staying active. This reduction can offset 200 to 300 calories daily, effectively shrinking or eliminating your calorie deficit without you realizing it.
The fix is deliberate. Set a daily step goal of 7,000 to 10,000. Walk after meals. Take phone calls standing up. Park at the far end of the lot. These additions seem minor individually, but they collectively create a meaningful increase in daily energy expenditure that can push you past a plateau.
Step 5: Address Sleep and Stress
If you’re sleeping fewer than seven hours a night consistently, your hormonal environment is actively working against fat loss. Short sleep raises ghrelin (hunger), lowers leptin (fullness), spikes cortisol (fat storage, especially abdominal), and increases cravings for calorie-dense foods. It can partially override semaglutide’s appetite-suppressing effects, making your deficit harder to maintain.
Chronic stress produces a similar hormonal profile through sustained cortisol elevation. You don’t need to eliminate stress entirely (that’s not realistic). But if your stress levels have increased meaningfully since starting treatment, through work, relationships, health concerns, or life changes, that could be a factor in your plateau.
Practical fixes: establish a consistent sleep schedule, make your bedroom cool and dark, cut caffeine after noon, and build even short recovery periods into high-stress days. These adjustments aren’t glamorous, but they create a hormonal environment that supports fat loss rather than fighting it.
Step 6: Get Updated Bloodwork
If you’ve addressed diet, exercise, sleep, and dosing and your plateau persists beyond six weeks, medical factors need to be investigated. Conditions that commonly interfere with weight loss include hypothyroidism, worsening insulin resistance, PCOS, and cortisol disorders.
Request a comprehensive panel from your provider: TSH and free T4 (thyroid), fasting glucose, fasting insulin, HbA1c, and cortisol if symptoms warrant it. These tests are simple and can identify problems with straightforward solutions. Hypothyroidism, for example, is treated with a daily pill and can remove a significant metabolic barrier once addressed.
Also review your current medication list. Corticosteroids, certain antidepressants, beta-blockers, gabapentin, and some diabetes drugs promote weight gain and can counteract semaglutide’s effects. Your provider may be able to switch to alternatives with a more neutral metabolic profile.
Step 7: Consider Switching to Tirzepatide
If you’ve maximized your semaglutide dose, optimized lifestyle factors, ruled out medical causes, and you’re still stuck, switching to tirzepatide may be the logical next step. Tirzepatide is a dual GIP/GLP-1 receptor agonist, meaning it works through an additional mechanism that semaglutide doesn’t target.
Head-to-head data suggests tirzepatide produces approximately 5% greater body weight loss on average compared to semaglutide at maximum doses. Some patients who plateau on semaglutide respond well to tirzepatide because of that second receptor pathway. The tirzepatide weight loss results break down the clinical data in detail.
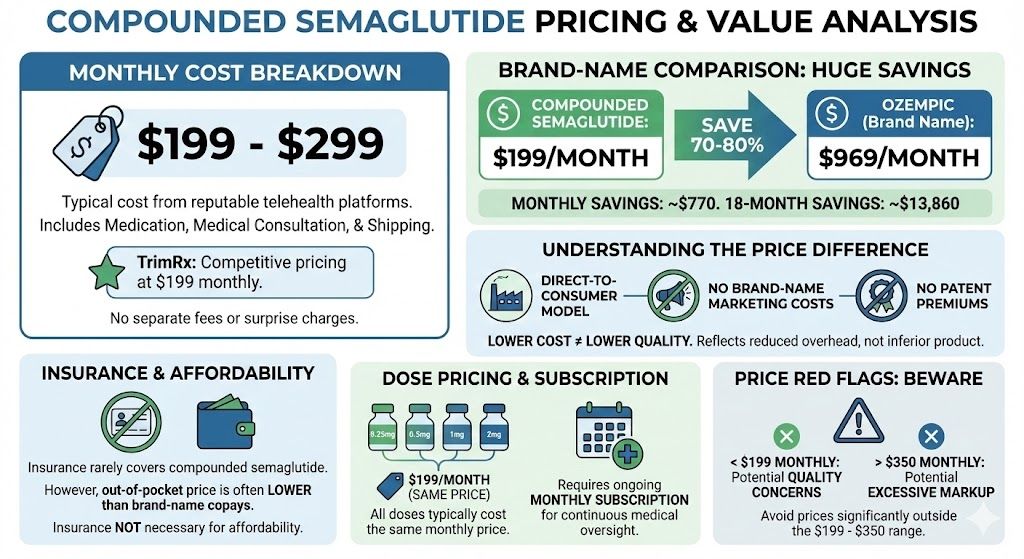
TrimRx offers both compounded semaglutide and compounded tirzepatide, with providers who can help determine whether staying the course with an adjusted approach or switching medications entirely is the better move for your situation.
Your Plateau Action Plan
Work through these steps in order:
Ask your provider about a dose increase if you’re not at the maximum. Track your food intake precisely for one week, including all beverages, oils, and incidental eating. Add resistance training two to three times weekly and increase daily steps to 7,000 to 10,000. Boost protein intake to at least 0.7 grams per pound of body weight. Fix sleep habits, aiming for seven or more hours nightly. Request updated bloodwork if your plateau persists beyond six weeks. Review all current medications for weight-promoting side effects. Discuss switching to tirzepatide if you’ve exhausted semaglutide’s dose range and lifestyle optimization.
A plateau doesn’t mean your weight loss journey is over. It means the approach that got you here needs updating to get you to the next phase. Most people who work through these steps systematically find that progress resumes within a few weeks.
This information is for educational purposes and is not medical advice. Consult with a healthcare provider before starting any medication. Individual results may vary.

Transforming Lives, One Step at a Time
Keep reading
How Long Can You Take Semaglutide?
There is no established maximum duration for semaglutide use. Whether you’re taking brand-name Ozempic, Wegovy, or compounded semaglutide, the medication is designed for long-term,…
Semaglutide to Tirzepatide: Switching Guide
Switching from semaglutide to tirzepatide is one of the most clinically supported medication transitions in GLP-1 weight loss treatment. You’re moving from a single-receptor…
Semaglutide First Week: What Happens to Your Body
Your first week on semaglutide probably won’t bring dramatic weight loss, and that’s completely by design. The starting dose of 0.25 mg is intentionally…



