Stopping Ozempic: What Happens and How to Manage Weight Regain

If you’re taking Ozempic and wondering what happens when you stop—whether you’ve reached your goal weight, can’t tolerate the side effects, or are stopping for other reasons—you deserve honest information beyond vague warnings about “possibly regaining weight.”
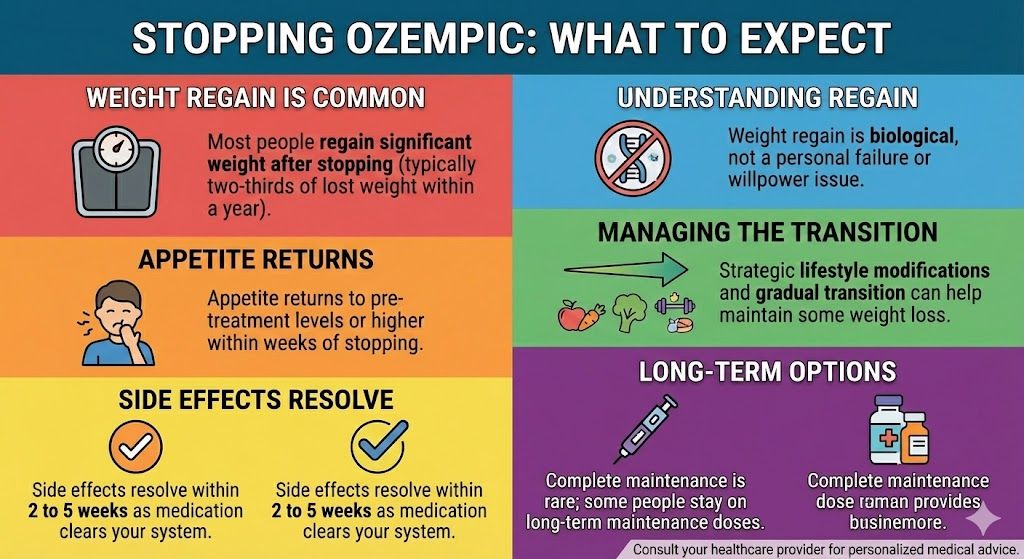
Here’s the reality: most people experience significant weight regain after stopping Ozempic. Clinical studies show that participants regained approximately two-thirds of the weight they lost within one year of discontinuing treatment. This isn’t a personal failure or lack of willpower. It’s a biological response to the removal of medication that was fundamentally altering your appetite signals and metabolism. However, weight regain isn’t inevitable or uniform. With strategic planning, lifestyle modifications, and realistic expectations, many people successfully maintain substantial portions of their weight loss after stopping.
This guide explains exactly what to expect when stopping Ozempic, why weight regain happens, proven strategies to minimize it, how to transition off the medication properly, and realistic long-term expectations for weight maintenance.
Key Takeaways: Stopping Ozempic
- Most people regain significant weight after stopping (typically two-thirds of lost weight within a year)
- Appetite returns to pre-treatment levels or higher within weeks of stopping
- Side effects resolve within 2 to 5 weeks as medication clears your system
- Weight regain is biological, not a personal failure or willpower issue
- Strategic lifestyle modifications can help maintain some weight loss
- Complete maintenance of all lost weight is rare but partial maintenance is achievable
- Transitioning gradually rather than stopping abruptly may help
- Some people choose to stay on long-term maintenance doses
What Happens Immediately After Stopping Ozempic
Understanding the timeline of changes helps you prepare and respond appropriately.
Week 1: Minimal Changes
During the first week after your last dose, you’ll likely notice minimal changes. Semaglutide has a long half-life of about 7 days, meaning after one week, roughly half the medication remains in your system. You’ll still experience some appetite suppression, though it might feel slightly less intense. Side effects like nausea or digestive issues continue if you were experiencing them. Weight remains stable or continues declining slightly from momentum.
Many people feel encouraged during this first week, thinking “maybe I won’t regain weight” or “my appetite has permanently changed.” Unfortunately, this early stability is temporary, reflecting medication still in your system rather than sustained behavioral changes.
Weeks 2 to 3: The Return of Appetite
This is when most people notice significant changes. Appetite returns, often stronger than you remember before treatment. Food thoughts increase dramatically—the “food noise” that disappeared on Ozempic comes roaring back. Portions that satisfied you on Ozempic no longer feel adequate. Cravings intensify for foods you didn’t think about while on medication.
This appetite return can feel shocking and distressing. Many people describe feeling “out of control” or worry that something is wrong with them. These are normal responses as your body adjusts to the absence of GLP-1 medication suppressing appetite signals.
Side effects begin resolving during this period. Nausea improves significantly. Digestive function normalizes with faster gastric emptying. Energy levels often improve if fatigue was an issue.
Weeks 3 to 5: Full Medication Clearance
By weeks 3 to 5, semaglutide is essentially eliminated from your system (5 half-lives = 97% clearance). Appetite reaches pre-treatment levels or potentially higher as your body attempts to restore lost weight. Hunger signals are strong and persistent. Satiety from meals is less durable—you feel hungry again sooner after eating.
Weight regain typically begins during this period, starting gradually then potentially accelerating. Initial regain of 2 to 5 pounds within the first month is common.
All side effects have resolved completely by this point. Your digestive system returns to normal speed. Nausea is gone. Bowel function normalizes.
Month 2 and Beyond: The New Normal
After about 2 months, your body has fully adjusted to the absence of medication. This is your post-Ozempic baseline. Appetite and hunger are stable at pre-treatment levels or somewhat elevated. Metabolic rate may be slightly reduced if you lost significant muscle mass during treatment. Food obsession may return if it was an issue before treatment.
Weight trajectory depends on your behaviors and strategies implemented during this adjustment period.
For detailed information about medication clearance, see our guide to how long semaglutide stays in your system.
The Reality of Weight Regain: What Studies Show
Understanding the data helps set realistic expectations rather than false hope.
The STEP 1 Extension Study
The most comprehensive data comes from the STEP 1 trial extension. Participants who lost an average of 17.3% of their body weight over 68 weeks on semaglutide 2.4 mg then stopped treatment. After one year off medication, they regained an average of 11.6% of their starting body weight (about two-thirds of what they lost).
Breaking this down: if someone weighed 250 pounds, lost 43 pounds (17.3%) to reach 207 pounds, they regained approximately 29 pounds within a year, ending around 236 pounds. They maintained only about one-third of their total weight loss.
Individual Variation
While the average is two-thirds regain, individual results vary tremendously. Some people regained 100% of lost weight within months. Others maintained 50% or more of their loss. A small percentage maintained most or all of their weight loss.
Factors predicting better maintenance included sustained lifestyle changes in diet and exercise, regular physical activity including resistance training, higher protein intake, continued dietary monitoring and awareness, psychological support or counseling, and realistic expectations rather than “diet mentality.”
Why Complete Maintenance Is Rare
Very few people maintain 100% of their Ozempic weight loss after stopping. This isn’t because people are weak or lack discipline. The biological reality is that your body’s set point defending mechanisms remain active. Appetite regulation returns to baseline. The metabolic advantages from GLP-1 activation disappear. Food reward pathways return to normal sensitivity.
Ozempic was doing significant biological heavy lifting that lifestyle factors alone typically can’t replicate completely.
What “Success” Looks Like
Given these realities, redefining success helps maintain perspective. Maintaining 30% to 50% of total weight loss is a realistic and meaningful achievement. For example, losing 50 pounds on Ozempic and maintaining 15 to 25 pounds off represents genuine success, improving health markers and quality of life compared to pre-treatment weight.
Preventing complete regain back to starting weight or higher is another success metric. Even regaining some weight while staying below your starting point provides health benefits.
Why Weight Regain Happens: The Biology
Understanding the biological mechanisms helps you respond strategically rather than blaming yourself.
Appetite Hormone Changes
GLP-1 medications suppress appetite by activating receptors throughout your digestive system and brain. When you stop, these effects disappear. Ghrelin (hunger hormone) increases back to or above baseline levels. GLP-1 (natural satiety hormone) returns to normal lower levels. Leptin (satiety hormone) may be reduced if you lost significant fat mass. Peptide YY and other satiety signals normalize.
The net effect is increased hunger with decreased satiety—a perfect storm for weight regain.
Metabolic Adaptation
When you lose significant weight, your body adapts metabolically in ways that promote regain. Your metabolic rate decreases beyond what would be expected from lost body mass alone. This adaptive thermogenesis means you burn fewer calories at your new lower weight than someone who was always that weight. Energy expenditure from physical activity decreases (you naturally move less without realizing it). Efficiency of muscular work improves (muscles burn fewer calories doing the same activities).
These adaptations can persist for years after weight loss, making maintenance challenging.
Set Point Defense
Your body has a defended weight range or “set point” influenced by genetics, previous maximum weight, and other factors. When weight drops below this range, biological systems activate to restore it. Hunger increases, satiety decreases, metabolic rate slows, and food becomes more rewarding and appealing.
These aren’t conscious changes you can simply override with willpower. They’re automatic biological responses designed to prevent starvation (which your body interprets significant weight loss as, regardless of your starting point).
Loss of Medication-Specific Benefits
Ozempic provides benefits beyond just appetite suppression that contribute to weight loss. Slowed gastric emptying makes smaller meals more satisfying. Reduced food noise and cravings decrease impulse eating. Potential effects on food reward pathways reduce hedonic eating. These benefits disappear when you stop, removing multiple mechanisms that were supporting weight maintenance.
Psychological Factors
The psychological transition off Ozempic also matters. Many people feel less supported or accountable without regular medication and appointments. The fear of regain creates anxiety that can paradoxically worsen eating patterns. Loss of the “tool” that made weight control feel manageable can feel demoralizing. Some people adopt an “all or nothing” mentality where any regain triggers complete abandonment of healthy habits.
These psychological responses compound the biological challenges.
For comprehensive information about Ozempic treatment, see our complete guide to Ozempic for weight loss.
Common Reasons People Stop Ozempic
Understanding why people discontinue helps contextualize your own decision.
Reached Goal Weight
Some people reach their target weight and want to try maintaining without medication. This is understandable, but it’s important to recognize that reaching a goal weight doesn’t mean the underlying biological factors driving obesity have resolved. Many people find that maintenance requires ongoing treatment.
Side Effects
Intolerable nausea, vomiting, or gastrointestinal issues cause some people to stop despite good weight loss results. Persistent fatigue that doesn’t improve may make treatment unsustainable. Severe constipation unresponsive to interventions can be debilitating. For some, the quality of life impact from side effects outweighs the benefits of weight loss.
Cost
Brand-name Ozempic costs $900 to $1,000+ monthly without insurance. Insurance coverage is inconsistent, particularly for weight loss versus diabetes indications. When coverage ends or changes, the cost becomes prohibitive for many people. Some people lose access to affordable compounded versions due to supply issues or regulatory changes.
Pregnancy Planning
Women planning to become pregnant must stop Ozempic at least 2 months before attempting conception. This medically necessary discontinuation forces weight maintenance without medication support during a critical time.
Medical Reasons
Development of pancreatitis, gallbladder problems, or other complications requires discontinuation. Some people develop thyroid concerns (though the human risk appears very low). Preparation for surgery sometimes requires temporarily stopping.
Personal Choice
Some people feel uncomfortable taking medication long-term for weight management. Others want to prove to themselves they can maintain weight without pharmaceutical help. Life changes or shifting priorities sometimes lead people to discontinue.
Lost Effectiveness
A small percentage of people find Ozempic loses effectiveness over time (though true tolerance is rare). When weight loss plateaus despite maximum doses, some people choose to stop rather than continuing expensive treatment without results.
Strategies to Minimize Weight Regain
While some regain is likely, these evidence-based strategies help minimize it.
Transition Gradually, Not Abruptly
Instead of stopping cold turkey, consider a gradual taper. Drop to a lower dose for 1 to 2 months before stopping completely. For example, if you’re on 2 mg weekly, drop to 1 mg for a month, then 0.5 mg for a month, then stop. Some people maintain on the lowest dose (0.25 mg) long-term as a compromise.
Gradual reduction allows your appetite to return more slowly, giving you time to adjust habits. It prevents the shock of sudden full appetite return.
Prioritize Protein Aggressively
High protein intake is the single most important dietary factor for maintaining weight loss. Aim for 0.8 to 1 gram per pound of goal body weight daily (or 1.2 to 1.6 g/kg). Protein provides the most satiety per calorie of any macronutrient. It supports muscle mass preservation which maintains metabolic rate. It has the highest thermic effect (burns more calories during digestion).
Make protein the foundation of every meal and snack. This becomes even more critical when appetite-suppressing medication is removed.
Implement Resistance Training
Building or preserving muscle mass is crucial for long-term maintenance. Muscle tissue burns more calories at rest than fat tissue. More muscle means a higher metabolic rate. Resistance training improves body composition even if weight increases slightly (muscle weighs more than fat).
Train all major muscle groups 2 to 4 times weekly. Progressive overload (gradually increasing weight/resistance) is key. Consider working with a trainer to optimize your program.
Continue Monitoring and Accountability
Self-monitoring prevents gradual weight creep from becoming significant regain. Weigh yourself weekly (same day, same time, same conditions). Track food intake at least occasionally to maintain awareness. Use photos or measurements to track changes beyond just weight. Consider regular appointments with a dietitian or health coach.
Accountability helps catch small gains before they become large ones.
Maintain Dietary Structure
Keep the eating patterns you developed on Ozempic even without appetite suppression enforcing them. Continue eating smaller, more frequent meals rather than huge portions. Keep following general healthy eating guidelines you learned. Avoid keeping trigger foods readily accessible at home. Plan meals in advance rather than deciding when hungry.
Structure compensates somewhat for reduced internal satiety signals.
Stay Extremely Active
Physical activity helps maintain weight loss more than it causes initial loss. Aim for 250 to 300 minutes of moderate activity weekly (this is higher than standard recommendations because you’re maintaining weight loss). Include both cardio and resistance training. Increase daily movement through walking, taking stairs, and active hobbies. Consider using a step counter and aiming for 10,000+ steps daily.
High activity levels help counteract metabolic adaptation.
Address Psychological Factors
Work with a therapist or counselor specializing in eating behaviors if applicable. Develop strategies for stress management that don’t involve food. Build support systems beyond medication (support groups, friends, family). Practice self-compassion rather than self-criticism around weight fluctuations. Focus on health behaviors you can control rather than just scale weight.
Psychological resilience helps you persist through challenges.
Consider Maintenance Medications
Some people successfully maintain on lower doses of Ozempic (0.25 to 0.5 mg weekly). Others transition to different weight management medications that might be better tolerated or less expensive. Metformin, naltrexone-bupropion, or phentermine might help some individuals. Discuss options with your provider if maintaining without medication proves too difficult.
Prepare for the Long Term
Understand that maintenance requires ongoing effort, likely for years or permanently. Weight regain isn’t a one-time event you prevent—it’s an ongoing pressure you manage. Having realistic expectations prevents discouragement. Plan for lifelong behavior changes rather than short-term fixes.
For strategies specific to maintaining results, see our month-by-month weight loss results guide.
How to Stop Ozempic Properly
If you’re stopping Ozempic, proper transition planning helps.
Discuss with Your Provider
Don’t stop Ozempic without involving your healthcare provider in the decision. They can help assess whether stopping is appropriate timing, develop a transition plan including tapering schedule, identify alternative approaches for diabetes management if applicable, set up monitoring for weight and health markers, and provide resources and referrals for ongoing support.
Collaborative planning improves outcomes compared to stopping independently.
Consider a Tapering Schedule
Work with your provider to develop a gradual reduction plan. A typical taper might be: if on 2 mg weekly, drop to 1 mg for 4 to 8 weeks, then drop to 0.5 mg for 4 to 8 weeks, then drop to 0.25 mg for 4 to 8 weeks, then stop or maintain on 0.25 mg long-term.
The exact schedule depends on your individual situation, how much weight you need to maintain, and how you respond to reductions.
Ramp Up Other Strategies Before Stopping
In the weeks before your last dose, intensify other maintenance strategies. Increase protein intake to target levels. Establish a consistent resistance training routine. Start tracking food intake again if you’d stopped. Schedule regular weigh-ins. Build meal planning habits. Connect with support resources.
Getting these systems in place while appetite is still suppressed sets you up better for when it returns.
Set Realistic Expectations
Understand that some weight regain is normal and expected, not a sign of failure. Define what “success” looks like for you (maintaining X pounds or X percentage of loss). Plan how much regain would prompt you to seek additional help or restart medication. Mentally prepare for appetite changes so they don’t surprise and overwhelm you.
Plan for the First Three Months Carefully
The first three months after stopping are critical. This is when appetite returns strongest and weight regain risk is highest. Consider scheduling extra accountability check-ins during this period. Avoid major stressful events or changes if possible. Be extra diligent with monitoring and maintenance behaviors. Have a plan for what you’ll do if regain exceeds your predetermined threshold.
Extra support during this transition period pays dividends long-term.
Know Your Restart Criteria
Decide in advance what circumstances would make you consider restarting Ozempic or trying an alternative medication. Some reasonable criteria might be regaining more than 50% of lost weight, weight regain causing return of comorbidities (diabetes, sleep apnea, etc.), or inability to maintain behaviors without medication support despite best efforts.
Having predetermined criteria prevents reactive decision-making and helps you restart if needed without feeling like you’ve failed.
Alternatives If Stopping Due to Specific Issues
If you’re stopping Ozempic because of problems rather than achieving goals, alternatives might exist.
If Stopping Due to Side Effects
Consider trying a different GLP-1 medication. Some people tolerate tirzepatide (Mounjaro/Zepbound) better than semaglutide despite similar mechanisms. Liraglutide (Saxenda) requires daily injections but has different pharmacokinetics. Staying at a lower Ozempic dose with manageable side effects might be better than stopping completely.
Try aggressive side effect management before discontinuing. Use anti-nausea medications, adjust diet, address constipation proactively, and optimize injection timing and technique.
Discuss whether temporary discontinuation with plan to retry after a break might work.
For detailed side effect management, see our comprehensive semaglutide side effects guide.
If Stopping Due to Cost
Explore compounded semaglutide options if not already using them. Compounded semaglutide at $199 monthly through TrimRx is significantly more affordable than brand-name options. Look into patient assistance programs for brand-name medications. Consider whether staying on the lowest effective dose reduces cost enough to continue. Explore insurance appeals or changing insurance plans during open enrollment.
Sometimes even a minimal dose provides enough benefit to make continuation worthwhile financially.
If Stopping Due to Plateau
Before stopping due to lack of continued progress, verify you’re at the maximum dose (2 mg weekly for Ozempic). Consider whether 4 to 6 more weeks at maximum dose might break the plateau. Evaluate whether dietary factors or decreased activity explain the plateau rather than medication failure.
Discuss switching to tirzepatide, which shows better average weight loss than semaglutide. Some people who plateau on one GLP-1 medication see renewed progress on another.
For comparison of options, see our Mounjaro vs Ozempic guide.
If Stopping for Pregnancy
This is a necessary medical discontinuation requiring the full 2-month washout. Focus on maintaining weight during washout and pregnancy rather than losing more. Work with your OB/GYN on appropriate pregnancy weight management. Plan to resume treatment after delivery and breastfeeding if desired.
For complete information, see our guide to Ozempic and pregnancy.
Long-Term Maintenance: Realistic Expectations
Setting realistic long-term expectations helps maintain perspective and motivation.
Maintenance Is Active, Not Passive
Weight maintenance after loss requires ongoing effort and vigilance. It’s not something you achieve once and forget about. Successful maintainers report that they think about food choices most days, stay physically active consistently, monitor weight and behaviors regularly, and adjust strategies when they notice weight creeping up.
This isn’t a depressing reality—it’s simply honest. Knowing this helps you prepare mentally.
You May Need More Support Than Before Weight Loss
Counterintuitively, maintaining weight loss often requires more ongoing effort than maintaining your original higher weight. This isn’t fair, but it reflects biological reality. The metabolic adaptations and appetite changes that promote regain persist for years.
Building support systems that acknowledge this reality helps sustain motivation.
Some Regain Doesn’t Mean Complete Failure
Regaining 10 or 15 pounds doesn’t negate losing 50 pounds. You’re still meaningfully healthier than at your starting weight. Each pound of maintained loss provides health benefits. The “all or nothing” mentality where any regain equals complete failure sabotages long-term success.
Practice self-compassion and focus on overall trajectory rather than perfection.
Consider Long-Term Low-Dose Medication
There’s increasing recognition that obesity is a chronic disease often requiring long-term treatment. Staying on a low maintenance dose of Ozempic (0.25 or 0.5 mg weekly) long-term is a reasonable strategy for many people. This is analogous to treating other chronic conditions like diabetes or hypertension—ongoing treatment maintains beneficial results.
The “take medication temporarily to lose weight then maintain without it” model doesn’t work well for most people. Accepting that long-term or indefinite treatment might be necessary isn’t failure—it’s realistic medical management.
Regular Reassessment
Schedule regular check-ins with your healthcare provider every 3 to 6 months to reassess weight trajectory, evaluate maintenance strategies, adjust approaches as needed, and monitor for any health changes.
Ongoing medical involvement supports long-term success better than trying to manage independently.
Frequently Asked Questions
What happens when you stop taking Ozempic?
When you stop Ozempic, appetite returns to pre-treatment levels within 2 to 3 weeks as the medication clears your system. Most people experience significant weight regain, typically two-thirds of lost weight within one year. Side effects like nausea and digestive issues resolve within 2 to 5 weeks. Hunger and food cravings increase substantially. Metabolic rate may be slightly reduced if you lost significant muscle during treatment. The speed of gastric emptying returns to normal.
How much weight do you gain back after stopping Ozempic?
Clinical studies show people regain an average of two-thirds of their lost weight within one year of stopping. Individual results vary widely—some regain 100% while others maintain 50% or more of their loss. Factors affecting regain include lifestyle modifications made during treatment, protein intake and resistance training after stopping, ongoing dietary monitoring, and psychological support. Complete maintenance of all lost weight is rare but partial maintenance is achievable with strategic effort.
Can you stop Ozempic cold turkey?
Yes, you can stop Ozempic abruptly without dangerous withdrawal symptoms or medical complications. However, gradual tapering may help minimize weight regain by allowing your appetite to return more slowly and giving you time to adjust habits progressively. Tapering from a higher dose to progressively lower doses over several months before stopping completely can make the transition more manageable for some people.
How long does it take for Ozempic to get out of your system?
Semaglutide has a half-life of approximately 7 days. After your last dose, it takes about 5 weeks (5 half-lives) for 97% of the medication to be eliminated from your system. Effects on appetite suppression begin diminishing within 1 to 2 weeks and are largely gone by 3 to 4 weeks. Side effects typically resolve within 2 to 5 weeks. Complete medication clearance occurs by about 5 to 6 weeks after your last injection.
Will I regain all the weight I lost on Ozempic?
Not necessarily, but significant regain is common. Studies show average regain of two-thirds of lost weight within one year, but individual results vary tremendously. Some people regain everything while others successfully maintain 50% or more of their loss. Strategic lifestyle modifications including high protein intake, resistance training, ongoing dietary monitoring, and regular physical activity can help minimize regain. Complete maintenance is rare but partial maintenance is realistic and meaningful.
How do I stop Ozempic without gaining weight?
While completely preventing weight regain is difficult, you can minimize it by tapering gradually instead of stopping abruptly, prioritizing protein (0.8 to 1g per pound of body weight daily), implementing consistent resistance training 2 to 4 times weekly, continuing to monitor food intake and body weight, staying highly active (250+ minutes weekly), maintaining eating patterns developed during treatment, and potentially staying on a low maintenance dose long-term. Understand that some regain is biologically likely despite best efforts.
Can you restart Ozempic after stopping?
Yes, you can restart Ozempic after stopping. If you regain significant weight, develop side effects that later resolve, or initially stopped for temporary reasons like pregnancy, restarting is medically acceptable. When restarting, you’ll need to begin at the starting dose (0.25 mg) and gradually titrate up again following the standard dosing schedule. You cannot restart at your previous higher dose immediately. Discuss restarting with your healthcare provider to ensure it’s appropriate for your situation.
What are the withdrawal symptoms from Ozempic?
Ozempic doesn’t cause true withdrawal symptoms like addictive substances. However, you’ll experience the return of appetite and hunger as the medication clears your system, increased food cravings and “food noise,” potential emotional distress about these changes, and resolution of side effects (which is positive). Some people describe feeling out of control with eating as appetite returns, but this is your baseline appetite returning rather than withdrawal. There are no dangerous medical complications from stopping.
Should I taper off Ozempic or stop suddenly?
Tapering is generally preferable to sudden discontinuation for most people. Gradual reduction allows appetite to return more slowly, gives you time to adjust eating habits progressively, makes the transition feel more manageable psychologically, and may reduce overall weight regain. A typical taper drops one dose level every 4 to 8 weeks. However, some situations require immediate discontinuation (pregnancy, serious side effects), which is medically safe to do. Discuss the best approach with your healthcare provider.
How can I maintain my weight after stopping Ozempic?
Maintaining weight requires ongoing effort including eating high protein at every meal (0.8 to 1g per pound body weight daily), resistance training 2 to 4 times weekly to preserve muscle, staying highly active (250+ minutes of moderate activity weekly), continuing to monitor food intake and weight regularly, maintaining meal patterns and portion sizes from treatment, avoiding gradual portion creep, building strong support systems, and managing stress through non-food methods. Consider staying on a low maintenance dose if maintaining without medication proves too difficult. Work with healthcare providers for ongoing support.
Making Peace with the Reality of Stopping Ozempic
Stopping Ozempic requires realistic expectations, strategic planning, and self-compassion. The biological reality is that most people will regain significant weight after discontinuing treatment, not because of personal failure but because of powerful biological mechanisms defending against sustained weight loss. Understanding this reality helps you prepare appropriately rather than being blindsided by changes you weren’t expecting.
Success after stopping Ozempic doesn’t mean maintaining 100% of your weight loss—it means maintaining a meaningful portion of it through sustained lifestyle modifications, preventing complete regain to your starting weight or higher, improving health markers even if weight increases somewhat, and developing a sustainable relationship with food and exercise.
For many people, the most realistic approach involves either staying on a low maintenance dose of Ozempic indefinitely (treating obesity as the chronic condition it is), accepting that some weight regain is normal and expected while minimizing it through strategic efforts, or being willing to restart treatment if regain exceeds predetermined thresholds.
Whether you’re using brand-name Ozempic or more affordable compounded semaglutide at $199 monthly through TrimRx, the decision about when and whether to stop should involve careful consideration of your individual circumstances, goals, and capacity for maintenance. Get started with or continue comprehensive medical support that includes honest discussions about stopping, long-term maintenance strategies, and realistic expectations for life after medication.

Transforming Lives, One Step at a Time
Keep reading
Online Ozempic Prescription Texas
You can get an Ozempic prescription online in Texas through a licensed telehealth provider without an in-person visit. Texas telehealth law allows providers to…
Online Ozempic Prescription California
You can get an Ozempic prescription online in California through a licensed telehealth provider without an in-person visit. California’s telehealth laws allow providers to…
Weight Loss Clinic Online Texas: Your Options
An online weight loss clinic in Texas gives you access to GLP-1 medications like semaglutide and tirzepatide through a fully virtual process. You complete…



