Why Am I Not Losing Weight on Zepbound? 7 Reasons

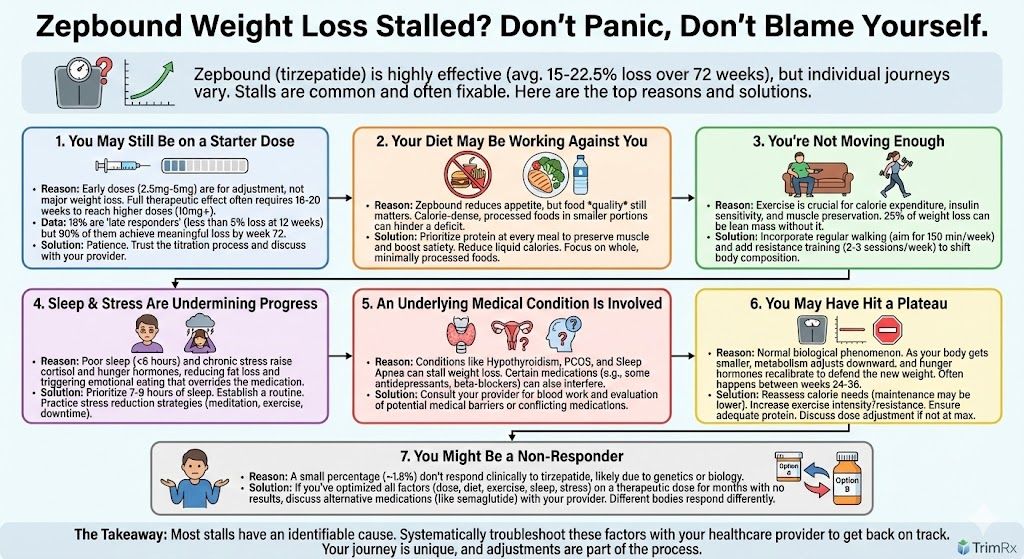
You started Zepbound expecting significant weight loss, but the scale isn’t cooperating. Maybe you’ve lost a little and then stalled, or maybe you haven’t seen much change at all. Either way, you’re wondering what’s going wrong.
Here’s the reassuring news: most people who don’t see early results on Zepbound still go on to lose meaningful weight if they stay the course and address the right factors. A post hoc analysis of the SURMOUNT-1 trial found that 90% of “late responders” (people who hadn’t lost 5% of their body weight by week 12) eventually achieved clinically significant weight loss by week 72.
So before you conclude that Zepbound isn’t working, let’s look at the seven most common reasons weight loss stalls and what you can do about each one.
1. You Haven’t Reached a Therapeutic Dose Yet
This is the most common reason people aren’t seeing results, and it’s also the most straightforward to address: you simply need more time.
Zepbound’s dosing schedule starts at 2.5 mg weekly, which is essentially a warm-up dose to let your body adjust. The dose increases by 2.5 mg every four weeks, meaning it takes 20 weeks to reach the maximum 15 mg dose if you’re titrating all the way up. Many people don’t experience substantial appetite suppression or weight loss until they hit 7.5 mg, 10 mg, or higher.
If you’ve been on Zepbound for less than four months, you may simply not have reached the dose where the medication works best for your body. The SURMOUNT-1 data showed that participants on 15 mg lost significantly more weight than those on 5 mg (22.5% vs. 16% of body weight), so dose matters.
What to do: Be patient through the titration phase. If you’re tolerating the current dose well and your provider agrees, continue escalating as scheduled. The average late responder in the clinical trial took about 25 weeks to hit the 5% weight loss threshold.
2. Your Calorie Intake Is Higher Than You Think
Zepbound works by reducing appetite, slowing gastric emptying, and decreasing food cravings. For most people, this naturally leads to eating less. But “eating less” doesn’t guarantee a calorie deficit, especially if the foods you’re choosing are calorie-dense.
Let’s say the medication cuts your portion sizes in half. If your previous meal was a 1,200-calorie plate, you’re now eating 600 calories per meal. Great. But if that smaller portion is mostly fried food, cheese, or sugar-heavy items, you could still be consuming more than your body needs to lose weight.
Common calorie culprits people overlook include beverages (specialty coffees, smoothies, alcohol, juice, soda), cooking oils and sauces, nuts and nut butters (healthy but very calorie-dense), and “healthy” snacks that are still high-calorie.
What to do: Try tracking your food intake for one to two weeks using an app. You don’t need to count calories forever, but a short tracking period often reveals surprising patterns. Focus on building meals around protein, vegetables, and whole grains while minimizing liquid calories and heavily processed foods.
3. You’re Not Getting Enough Protein
This one deserves its own category because inadequate protein is both common and consequential. When you’re losing weight, your body doesn’t just shed fat. It also loses some lean muscle mass. Clinical data from the SURMOUNT-1 body composition substudy found that about 25% of weight lost on tirzepatide came from lean mass rather than fat.
Losing muscle is problematic for several reasons. Muscle is metabolically active tissue, meaning it burns calories even at rest. The more muscle you lose, the more your metabolism slows, making continued weight loss harder. Low protein intake accelerates this muscle loss.
What to do: Aim for 0.7 to 1 gram of protein per pound of your goal body weight daily. For someone targeting 160 pounds, that’s roughly 110 to 160 grams of protein per day. Good sources include chicken, fish, eggs, Greek yogurt, cottage cheese, legumes, and tofu. Spreading protein across all meals (rather than loading it into one) helps with absorption and satiety.
4. You’re Sedentary
Exercise isn’t the primary driver of weight loss (diet is), but physical activity plays a supporting role that’s hard to replicate any other way. Movement increases your daily calorie expenditure, improves insulin sensitivity, supports better sleep, and helps preserve the lean muscle mass we just discussed.
Resistance training is particularly valuable. Lifting weights, using resistance bands, or doing bodyweight exercises two to three times per week sends signals to your body that it needs to hold onto muscle tissue, which shifts more of your weight loss toward fat.
Cardiovascular exercise (walking, cycling, swimming) contributes too, mainly by increasing your overall calorie burn and improving cardiovascular health.
What to do: Start with 150 minutes of moderate activity per week (like brisk walking) if you’re not currently active. Add resistance training two to three times weekly, focusing on major muscle groups. You don’t need a gym membership; bodyweight exercises like squats, lunges, push-ups, and planks are effective starting points.
5. Sleep Deprivation Is Working Against You
Poor sleep is one of the most underrated barriers to weight loss. When you don’t get enough quality sleep, your body produces more ghrelin (the hunger hormone) and less leptin (the satiety hormone). Cortisol rises, insulin sensitivity drops, and your brain’s reward centers become more responsive to high-calorie foods.
Research consistently shows that people who sleep fewer than six hours per night have a significantly harder time losing weight and are more likely to regain weight they’ve lost. This happens even when calorie intake is controlled, meaning sleep deprivation appears to directly affect how your body metabolizes and stores energy.
Zepbound can’t fully override these hormonal disruptions. If you’re chronically underslept, you may experience stronger cravings and less appetite suppression than you would with adequate rest.
What to do: Prioritize seven to nine hours of sleep per night. Establish a consistent sleep schedule (same bedtime and wake time, even on weekends), limit caffeine after early afternoon, reduce screen time before bed, and keep your bedroom cool and dark. If you suspect you have sleep apnea (symptoms include snoring, daytime fatigue, and waking up unrefreshed), talk to your provider about a sleep study.
6. Chronic Stress Is Sabotaging Your Progress
Stress affects weight loss through multiple pathways. Elevated cortisol promotes fat storage, particularly visceral fat around the midsection. Stress also triggers emotional eating in many people, eating that’s driven by feelings rather than physical hunger, which can partially bypass the appetite suppression Zepbound provides.
Beyond the biological effects, stress often leads to behaviors that undermine weight loss: skipping workouts, making quick and less healthy food choices, drinking more alcohol, and sleeping poorly.
What to do: Identify your primary stressors and develop strategies to manage them. This might include regular exercise (which itself reduces stress hormones), meditation or deep breathing practices, therapy or counseling, setting boundaries at work, or building in daily downtime. The goal isn’t to eliminate stress entirely, but to develop better coping mechanisms that don’t revolve around food or inactivity.
7. An Underlying Medical Condition Is Interfering
Several medical conditions can slow or prevent weight loss even when medication and lifestyle factors are aligned.
Hypothyroidism slows your metabolism and can make weight loss extremely difficult. If you have unexplained fatigue, cold intolerance, dry skin, or constipation alongside weight loss resistance, ask your provider to check your thyroid function.
Polycystic ovary syndrome (PCOS) involves insulin resistance and hormonal imbalances that make weight loss challenging. GLP-1 medications like Zepbound can still work for people with PCOS, but results may be slower.
Insulin resistance and prediabetes can blunt weight loss responses, though tirzepatide is specifically designed to improve insulin sensitivity. People with type 2 diabetes typically lose less weight on GLP-1 medications than people without diabetes.
Medications can also interfere. Certain antidepressants (especially mirtazapine and some SSRIs), beta-blockers, corticosteroids, insulin, and some anticonvulsants are known to promote weight gain or make weight loss harder.
What to do: If you’ve addressed the lifestyle factors above and still aren’t seeing results, talk to your provider about testing for underlying conditions. Blood work to evaluate thyroid function, fasting insulin, and metabolic markers can identify treatable issues. If you’re on a medication that promotes weight gain, ask whether alternatives are available.
When to Reassess Your Treatment
There’s no hard cutoff for when Zepbound “should” be working, but general guidelines suggest reassessment if you’ve been at a maintenance dose (10 mg or 15 mg) for at least 12 to 16 weeks without achieving at least 5% body weight loss, or if you were losing weight and have stalled for more than eight to ten weeks despite optimizing lifestyle factors.
At that point, your provider might consider adjusting your dose, evaluating for underlying conditions, or discussing whether switching to a different medication might be worth trying. Some people respond better to semaglutide than tirzepatide, or vice versa, so a medication change doesn’t mean failure.
If you’re working with TrimRx, your telehealth provider can help troubleshoot your results and adjust your plan accordingly. Compounded tirzepatide and semaglutide options are available at accessible price points, and consultations don’t require an in-person visit.
Ready to explore your options? Take the TrimRx intake quiz to get started.
This information is for educational purposes and is not medical advice. Consult with a healthcare provider before starting any medication. Individual results may vary.

Transforming Lives, One Step at a Time
Keep reading
Zepbound Not Working: Troubleshooting Your Weight Loss
If Zepbound doesn’t seem to be producing the weight loss you expected, the medication probably isn’t the issue. Zepbound contains tirzepatide, a dual GIP/GLP-1…
Not Losing Weight on Zepbound? Here’s What to Do
If you’ve been taking Zepbound and the scale isn’t moving the way you expected, you’re not alone, and you’re not necessarily doing anything wrong….
Zepbound Before and After: What Results to Expect
Zepbound (tirzepatide) produces some of the most dramatic before and after transformations of any weight loss medication available. Clinical trial data from the SURMOUNT-1…



