Will Insurance Cover Mounjaro for Prediabetes?

In most cases, insurance will not cover Mounjaro (tirzepatide) specifically for a prediabetes diagnosis. Mounjaro is currently FDA-approved only for type 2 diabetes, and its weight loss counterpart Zepbound is approved for obesity. Prediabetes falls into a gap between these two indications, which means coverage depends heavily on your specific plan, your BMI, and how your provider codes the prescription.
That’s the frustrating short answer. The longer answer involves some real workarounds that can get you covered, or at least get you access at a price you can manage. Let’s walk through how insurance decisions actually work for this situation and what your realistic options are.
Why Prediabetes Creates a Coverage Problem
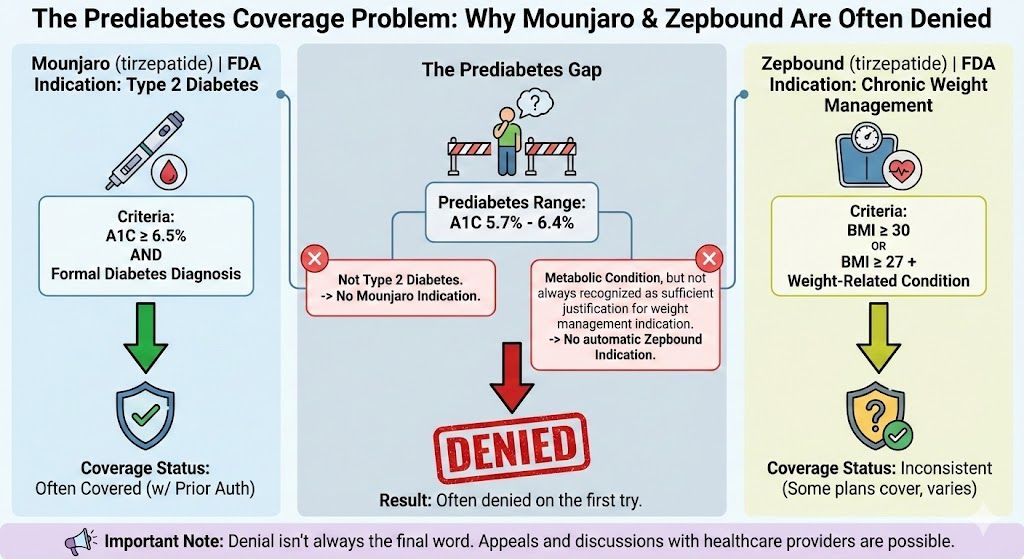
Insurance companies make coverage decisions based on FDA-approved indications. Here’s where Mounjaro sits right now:
Mounjaro (tirzepatide) is approved for type 2 diabetes. If your A1C is 6.5% or higher and you have a formal diabetes diagnosis, most commercial plans will cover it, often with prior authorization.
Zepbound (tirzepatide) is the same molecule approved for chronic weight management in adults with a BMI of 30 or above, or 27 or above with at least one weight-related condition. Some plans cover it, though weight loss medication coverage is still inconsistent across insurers.
Prediabetes (A1C between 5.7% and 6.4%) doesn’t qualify under either approval. You don’t have diabetes, so the Mounjaro indication doesn’t apply. And while prediabetes is a metabolic condition associated with excess weight, insurers don’t always recognize it as sufficient justification under the weight management indication.
The result is that prediabetes patients often get denied on the first try. But denial isn’t always the final word.
Paths to Getting Coverage
1. Qualify Through the Weight Management Indication
If your BMI is 30 or higher, or 27 or higher with a comorbidity like hypertension, high cholesterol, or sleep apnea, your provider may be able to prescribe Zepbound under the obesity indication instead. Prediabetes itself can sometimes count as a qualifying comorbidity for this pathway, depending on the insurer.
The key is how your provider documents and codes the prescription. A claim submitted with a primary diagnosis of obesity (ICD-10 code E66) and prediabetes as a secondary condition has a better chance than one coded primarily as prediabetes (R73.03).
2. Request Prior Authorization with Supporting Documentation
Even when initial claims are denied, a prior authorization request that includes your full metabolic profile can sometimes change the outcome. This typically means your provider submits:
- Your BMI and weight history
- A1C and fasting glucose levels showing prediabetes
- Documentation of failed lifestyle interventions (prior diet programs, exercise plans)
- Any additional metabolic risk factors (family history of diabetes, elevated triglycerides, hypertension)
- A letter of medical necessity explaining why pharmacological intervention is warranted before full diabetes develops
Some insurers respond to the preventive argument, especially when the cost of treating type 2 diabetes (which runs $10,000 to $15,000 annually on average) is weighed against the cost of preventing it. But this approach requires a provider willing to advocate on your behalf, and the success rate varies widely by plan.
3. Appeal a Denial
If your claim is denied, you have the right to appeal. First-level appeals are resolved internally by the insurance company. If that fails, an external appeal goes to an independent reviewer. According to data from state insurance departments, external appeals for medication denials are overturned in roughly 40 to 60% of cases, though this varies by state and situation.
The appeal process takes time, usually four to eight weeks. If you need the medication sooner, you may want to pursue other options in parallel.
4. Manufacturer Savings Programs
Eli Lilly (Mounjaro’s manufacturer) has offered savings cards that can reduce out-of-pocket costs for commercially insured patients. These programs change frequently, so check the current offers at the Mounjaro or Zepbound websites. Typically, these savings cards work best when your insurance covers the medication but leaves a high copay. They’re less helpful when the claim is denied outright.
What Each Insurance Type Typically Covers
Coverage patterns differ significantly depending on your type of insurance:
Commercial/employer plans have the most variation. Some progressive plans cover GLP-1 medications for weight management broadly. Others exclude weight loss drugs entirely. Your plan’s formulary and any specific obesity treatment exclusions determine what’s possible.
Medicare Part D generally does not cover medications prescribed for weight loss or obesity. However, recent legislative changes have opened the door for coverage of anti-obesity medications for Medicare beneficiaries. This is an evolving area, and coverage for prediabetes specifically remains limited. Mounjaro for a type 2 diabetes diagnosis is typically covered under Medicare.
Medicaid coverage varies by state. Some state Medicaid programs cover GLP-1 medications for weight management. Others don’t. Prediabetes as a standalone indication is rarely sufficient for Medicaid coverage.
Marketplace (ACA) plans follow similar patterns to commercial insurance. Coverage depends on the specific plan and formulary.
For a detailed breakdown of how these dynamics play out with semaglutide, our article on whether insurance covers Ozempic for prediabetes covers much of the same territory from the Ozempic side.
The Real Cost Without Insurance
If insurance isn’t an option, here’s what you’re looking at for brand-name tirzepatide:
Mounjaro without insurance runs approximately $1,000 to $1,200 per month at retail pharmacies. Zepbound is priced similarly. Discount cards through GoodRx or similar platforms can bring prices down somewhat, but rarely below $800 per month for brand-name versions.
For a full breakdown of those retail prices, our Mounjaro cost on GoodRx article covers current pricing in detail.
Those numbers put brand-name tirzepatide out of reach for many people paying out of pocket. Which brings us to the most practical alternative.
Compounded Tirzepatide: The Affordable Option
Compounded tirzepatide is the same active ingredient prepared by licensed compounding pharmacies. It’s available through telehealth providers at a fraction of the brand-name cost because it doesn’t carry the same pharmaceutical markup.
Through TrimRx, compounded tirzepatide starts at $179 per month. No insurance is needed. The process works like this: you complete an online consultation, a licensed provider reviews your health information and prescribes the medication if appropriate, and it ships directly to your door.
For prediabetes patients specifically, this route removes the insurance battle entirely. You don’t need to justify the indication to an insurer, wait for prior authorization, or file appeals. You work directly with a provider who evaluates whether the medication is right for your situation.
You can check your eligibility with a quick intake assessment.
Is Treating Prediabetes with Tirzepatide Worth It?
Let’s say a patient named Maria has an A1C of 6.3%, a BMI of 33, and a strong family history of type 2 diabetes. Her doctor has recommended lifestyle changes twice, and she’s lost some weight each time but regained it. She’s now considering tirzepatide.
From a pure cost perspective, treating prediabetes now is significantly less expensive than treating type 2 diabetes later. Diabetes management involves ongoing medication (often multiple drugs), regular lab monitoring, potential complications (kidney disease, neuropathy, cardiovascular events), and the cumulative health costs that come with a chronic progressive disease.
Tirzepatide for 12 to 18 months at $179 per month totals roughly $2,150 to $3,200. If that treatment helps Maria lose 15 to 20% of her body weight and return her A1C to normal range, the long-term savings, both financial and in quality of life, are substantial.
Research supports this approach. A 2023 study in the New England Journal of Medicine demonstrated that semaglutide 2.4 mg (a related GLP-1 medication) significantly reduced major cardiovascular events in adults with obesity, many of whom had prediabetes at baseline (Lincoff AM, et al., NEJM, 2023). While this study focused on semaglutide, the metabolic benefits of GLP-1 receptor agonists as a class are well established, and tirzepatide’s dual-agonist mechanism suggests at least comparable protective effects.
Steps to Take Right Now
If you have prediabetes and want to explore tirzepatide, here’s a practical action plan:
Check your insurance first. Call the number on your card and ask specifically whether Mounjaro or Zepbound is covered under your plan, and whether prediabetes or obesity qualifies. Get the answer in writing if possible.
Talk to your provider about coding. If you have a BMI that qualifies for the weight management indication, ask your doctor to code the prescription accordingly. This single step can make the difference between approval and denial.
Have a backup plan. If insurance won’t cooperate, compounded tirzepatide through a telehealth provider keeps the medication accessible. Don’t let an insurance denial delay treatment when your metabolic health is trending in the wrong direction.
Don’t wait for full diabetes. This sounds obvious, but many people do. They put off pharmacological treatment because prediabetes feels less urgent than a diabetes diagnosis. The whole point of catching it early is to act early. For a look at how tirzepatide works over time, our tirzepatide weight loss results article covers what the data shows.
Prediabetes is a window. Insurance makes it harder than it should be to climb through that window, but it’s not the only door. The medication is accessible, the evidence supports using it, and the cost of inaction is higher than the cost of treatment.
This information is for educational purposes and is not medical advice. Consult with a healthcare provider before starting any medication. Individual results may vary.

Transforming Lives, One Step at a Time
Keep reading
Mounjaro Cash Price: Your Options
Mounjaro without insurance costs approximately $1,050 to $1,200 per month at most retail pharmacies. That’s the cash price for a four-week supply regardless of…
Mounjaro Cost on GoodRx: Price Breakdown
Mounjaro (tirzepatide) on GoodRx typically costs between $950 and $1,100 per month depending on your dose and pharmacy, though prices fluctuate. That’s with a…
Mounjaro Starting Dose: Finding the Right Level
Mounjaro’s starting dose is 2.5 mg injected once weekly, and every patient begins here regardless of their weight, health goals, or prior medication history….



