GLP-1 vs. Lifestyle Changes: What Matters More?

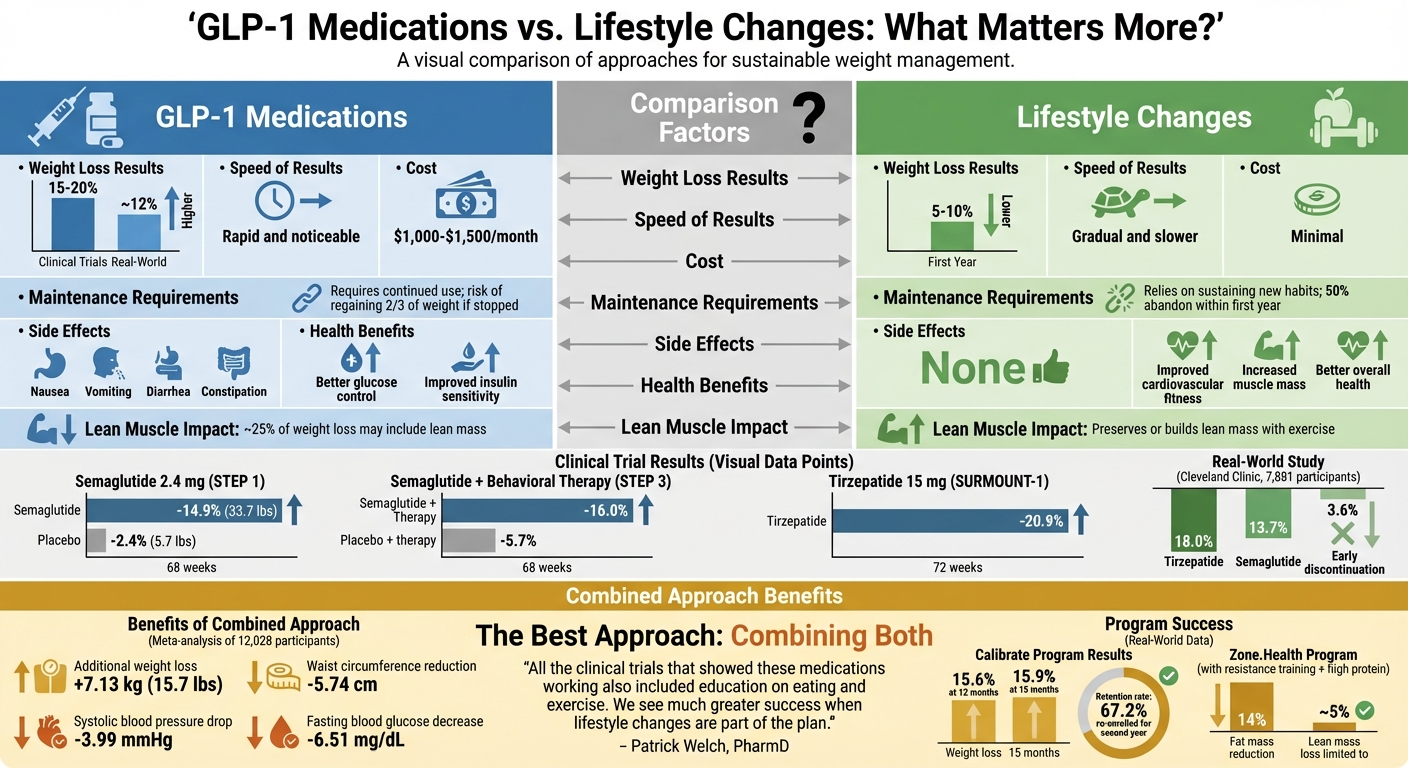
When it comes to weight loss, GLP-1 medications like Wegovy and Mounjaro are gaining attention for their ability to help people shed 15–20% of their body weight. However, lifestyle changes – including diet, exercise, and behavior adjustments – remain a key strategy, typically leading to 5–10% weight loss. The real question is: which approach works better?
Here’s the deal: GLP-1 medications can deliver faster and larger results but often require ongoing use and come with side effects like nausea and high costs (around $1,000–$1,500 per month). On the other hand, lifestyle changes are more affordable but harder to maintain long-term due to challenges like plateaus and emotional eating.
The best approach? A combination of both. Research shows pairing GLP-1 medications with lifestyle changes enhances results, improves overall health, and helps maintain weight loss more effectively.
Quick Comparison
| Factor | GLP-1 Medications | Lifestyle Changes |
|---|---|---|
| Weight Loss | 15–20% (clinical trials) | 5–10% (first year) |
| Cost | $1,000–$1,500/month | Minimal |
| Maintenance | Requires continued use | Relies on habit consistency |
| Side Effects | Nausea, GI issues, etc. | None |
| Health Benefits | Better glucose control | Improved fitness, muscle mass |
Bottom line: Combining GLP-1 medications with lifestyle adjustments offers the most effective path to sustainable weight loss.
GLP-1 Medications vs Lifestyle Changes: Complete Weight Loss Comparison
GLP-1 vs Lifestyle Weight Loss: What Works Better Long-Term?
How GLP-1 Medications Work for Weight Loss
GLP-1 medications work by targeting specific areas in the brain that regulate appetite and digestion. They influence receptors in the hypothalamus and brainstem, effectively reducing hunger signals. By activating neurons that suppress appetite and blocking those that stimulate it, these medications help curb the desire to eat. Additionally, they suppress dopamine release, which can lower food cravings and make calorie-dense foods less tempting.
Another key mechanism involves slowing down gastric emptying. Studies indicate that GLP-1 medications can delay this process by 23% to 27%, which helps you feel fuller for longer after eating. For instance, research on Semaglutide 2.4 mg shows it can reduce calorie intake by about 35%.
These drugs also play a role in regulating metabolism. They boost the body’s insulin response when glucose is present and suppress glucagon – a hormone that raises blood sugar. This dual action not only stabilizes blood sugar levels but also reduces hunger signals, contributing to weight loss and better metabolic health.
Tirzepatide takes this a step further. While Semaglutide focuses solely on GLP-1 receptors, Tirzepatide also activates GIP (glucose-dependent insulinotropic polypeptide) receptors. This combination improves how the body processes fats and enhances metabolic efficiency, which may explain its superior weight loss outcomes.
These mechanisms together explain the impressive results seen in clinical trials.
Clinical Results with GLP-1 Medications
The results from clinical studies highlight the effectiveness of GLP-1 medications for weight loss.
In the STEP 1 trial, 1,961 adults with a BMI of 30 or higher (or 27 with weight-related health conditions) took weekly doses of Semaglutide 2.4 mg for 68 weeks. Participants lost an average of 33.7 pounds, or 14.9% of their body weight, compared to just 5.7 pounds in the placebo group. The study, led by John Wilding, showed consistent outcomes across diverse groups.
When paired with intensive behavioral therapy, the results improve further. The STEP 3 trial involved 611 adults who combined Semaglutide 2.4 mg with behavioral counseling and a low-calorie diet. These participants achieved a 16.0% weight loss over 68 weeks – nearly triple the 5.7% weight loss seen in those who only received behavioral therapy and placebo.
Tirzepatide has shown even greater potential. In the SURMOUNT-1 trial, participants without diabetes taking the highest dose (15 mg) experienced an average weight loss of 20.9% over 72 weeks. Earlier GLP-1 medications like Liraglutide 3.0 mg (Saxenda) also delivered meaningful results, with an average weight loss of 18.5 pounds compared to 6.2 pounds for placebo over 56 weeks.
| Medication | Trial | Duration | Average Weight Loss | Placebo Weight Loss |
|---|---|---|---|---|
| Semaglutide 2.4 mg | STEP 1 | 68 weeks | 14.9% (33.7 lbs) | 2.4% (5.7 lbs) |
| Semaglutide 2.4 mg + Therapy | STEP 3 | 68 weeks | 16.0% | 5.7% |
| Tirzepatide 15 mg | SURMOUNT-1 | 72 weeks | 20.9% | Not specified |
| Liraglutide 3.0 mg | SCALE | 56 weeks | 8.4 kg (18.5 lbs) | 2.8 kg (6.2 lbs) |
While the results are promising, these medications do come with potential risks and side effects.
Side Effects and Medical Considerations
The most common side effects of GLP-1 medications are gastrointestinal issues, such as nausea, vomiting, diarrhea, and constipation. These symptoms are typically temporary and occur during the initial weeks as the dosage is gradually increased.
"While gastrointestinal side effects like nausea and constipation are common, they are usually temporary and manageable." – Dr. Chika Anekwe, Obesity Medicine Clinical Director at Massachusetts General Hospital Weight Center
Medical supervision is crucial when using these medications. Doctors usually start patients on a low dose, increasing it every four weeks to minimize side effects. They also monitor for rare but serious complications, including pancreatitis, gallbladder disease, and kidney problems. For example, in Liraglutide trials, 3.1% of participants developed gallbladder disease compared to 1.9% in the placebo group.
These medications are not suitable for everyone. They are contraindicated for individuals with medullary thyroid carcinoma or Multiple Endocrine Neoplasia type 2. Additionally, discontinuing the medication without maintaining significant lifestyle changes can lead to weight regain, as the body may respond by increasing hunger hormones like ghrelin.
The Role of Lifestyle Changes in Weight Loss
When it comes to shedding pounds, lifestyle changes – like improving your diet, committing to regular exercise, and using behavioral techniques – are at the heart of the process. The main idea is to create a caloric deficit, usually around 500 calories per day, while incorporating consistent physical activity and addressing the mental and emotional factors that influence eating habits. This method not only helps with weight loss but also boosts overall health.
These three elements work hand-in-hand to create lasting habits. Dietary changes focus on cutting calories while emphasizing high-protein and fiber-rich foods to help maintain muscle and keep you feeling full. Exercise recommendations typically include 150 to 300 minutes of moderate aerobic activity each week – think brisk walking or swimming – along with resistance training two or three times a week. Lastly, behavioral therapy, such as cognitive behavioral therapy (CBT) or mindfulness practices, helps tackle emotional eating and encourages long-term, healthy routines.
The benefits go beyond the number on the scale. Even modest weight loss can lead to lower blood pressure, better cholesterol levels, and improved blood sugar control. These health perks occur whether or not medications are part of the plan, underscoring the value of lifestyle adjustments for overall well-being.
Weight Loss Results from Lifestyle Changes
Lifestyle changes often lead to a 5–10% reduction in body weight within the first year. While this might seem modest compared to results achieved with medications, this level of weight loss has proven health benefits. It’s also a more sustainable approach, as extreme diets can lead to fatigue and nutrient deficiencies, which often result in failure over time.
A study published in JHEP Reports in 2025 followed 29 participants with liver disease over 12 weeks. It compared a lifestyle intervention involving a 500-calorie-per-day deficit with liraglutide treatment. Both groups achieved around 5% weight loss and saw similar reductions in liver fat and inflammation. This demonstrates that consistent lifestyle changes alone can yield clinically meaningful results.
The real challenge, however, is maintaining these results over time. Unlike tightly controlled clinical trials, real-life settings lack structured support, which often leads to lower adherence. While only 14–17% of participants drop out of clinical trials, approximately 50% of individuals abandon their programs within the first year in everyday circumstances.
Common Obstacles
Despite the clear benefits, sticking to lifestyle changes long-term can be tough due to several obstacles.
Weight loss plateaus can be particularly discouraging. As the body adjusts to a lower calorie intake, metabolism slows, making further weight loss harder without tweaking the plan.
Time constraints are another major issue. Meal prepping and maintaining a consistent workout routine require a significant time investment, which can feel overwhelming for those juggling work, family, and other responsibilities.
Muscle loss is a risk when calorie intake drops too low without adequate protein or strength training. High-protein diets combined with resistance exercises can help preserve muscle, but they require extra effort and planning.
Emotional eating is another hurdle. Stress, boredom, or other emotional triggers can lead to overeating, even when physical hunger isn’t a factor. Without addressing these underlying psychological challenges – through behavioral therapy or counseling – many struggle to stick with dietary changes. Additionally, biological factors like appetite hormones can make sustained weight loss even harder to achieve. These challenges highlight why combining lifestyle changes with other methods might be more effective for some individuals.
"Real life is different and results aren’t always as spectacular as in clinical trials." – Sarah Kim, MD, Professor of Medicine, University of California San Francisco
sbb-itb-e2779c3
GLP-1 Medications vs. Lifestyle Changes: Direct Comparison
Let’s break down the outcomes of GLP-1 medications and lifestyle changes side by side. This comparison can help you decide which approach – or combination – might work best for your goals. Each option has its own strengths and challenges, and results can vary widely depending on the individual.
The most striking difference lies in the speed and extent of weight loss. Clinical trials show that GLP-1 medications like semaglutide and tirzepatide can lead to a 15–20% weight reduction over 12–16 months, while diet and exercise typically result in 5–10% weight loss in the first year. For example, a Cleveland Clinic study from June 2025, involving 7,881 participants, found that high-dose tirzepatide users lost 18.0% of their body weight in one year, semaglutide users lost 13.7%, and those who discontinued early (within three months) lost just 3.6%.
"Our study shows that patients treated for obesity with semaglutide or tirzepatide lost less weight on average in a regular clinical setting compared to what is observed in randomized clinical trials."
- Hamlet Gasoyan, PhD, Researcher, Cleveland Clinic’s Center for Value-Based Care Research
Maintaining weight loss presents different challenges for each approach. GLP-1 medications require ongoing use to prevent regaining up to two-thirds of the lost weight. Interestingly, about half of users stop taking these medications within a year, a dropout rate similar to lifestyle programs. On the other hand, lifestyle changes demand consistent adherence to new habits, which can be equally challenging to sustain over time.
Here’s a quick breakdown of the key differences:
Comparison Table
| Factor | GLP-1 Medications | Lifestyle Changes |
|---|---|---|
| Speed of Results | Rapid and noticeable | Gradual and slower |
| Average Weight Loss | 15–20% (clinical trials); ~12% in real-world | 5–10% in the first year |
| Maintenance | Requires ongoing medication; risk of regain | Relies on sustaining new habits |
| Metabolic Benefits | Better glucose control and insulin sensitivity | Improved cardiovascular fitness and strength |
| Challenges | High cost ($1,000–$1,500/month), side effects (nausea, diarrhea), drug shortages | Time commitment, motivation, and plateaus |
| Lean Muscle Impact | ~25% of weight loss may include lean mass | Preserves or builds lean mass with exercise |
The financial aspect is another major consideration. GLP-1 medications cost between $1,000 and $1,500 per month without insurance, while lifestyle changes are generally more affordable. Additionally, GLP-1s offer benefits like improved glucose regulation, while lifestyle changes boost cardiovascular health and help maintain or even increase muscle mass.
Ultimately, neither approach is inherently better – it’s all about finding what aligns with your health needs, budget, and ability to stick with the plan long-term.
Combining GLP-1 Medications with Lifestyle Changes
Pairing GLP-1 medications with diet and exercise has been shown to improve appetite control, enhance insulin function, and support habits that lead to lasting results. Let’s dive into the research backing this combined approach.
Research on Combined Approaches
A 2025 meta-analysis of 33 randomized controlled trials, involving 12,028 participants, revealed that adding lifestyle changes to GLP-1 therapy resulted in an additional 7.13 kg (15.7 lbs) of weight loss, a reduction in waist circumference by 5.74 cm, a drop in systolic blood pressure by 3.99 mmHg, and a decrease in fasting blood glucose by 6.51 mg/dL. These findings highlight the enhanced benefits of combining medication with lifestyle adjustments.
Real-world data from the Calibrate telehealth program, published in October 2023, further supports this approach. Led by Dr. Donna Ryan, the study followed 2,643 participants using GLP-1 medications like semaglutide and liraglutide alongside structured lifestyle interventions. Participants experienced an average weight loss of 15.6% at 12 months, which increased slightly to 15.9% by 15 months. Notably, 67.2% of participants re-enrolled for a second year, indicating sustained engagement and success.
"A strategy combining exercise and liraglutide therapy improved healthy weight loss maintenance more than either treatment alone." – New England Journal of Medicine
Incorporating resistance training and a high-protein diet (1.2–1.5 g/kg of body weight daily) with GLP-1 therapy can also help preserve lean muscle mass. A June 2024 study on the Zone.Health program showed participants achieved a 14% reduction in fat mass, while limiting lean mass loss to about 5%.
How TrimRX Supports This Approach
TrimRX builds on this evidence by combining personalized GLP-1 therapy with tailored lifestyle plans to ensure long-term success. The program includes unlimited check-ins with medical professionals who adjust your nutrition and exercise strategies as you progress. With customized dosing and free home delivery, TrimRX makes it easier to stay consistent.
To further support your journey, TrimRX offers targeted supplements like the GLP-1 Daily Support ($119) for metabolic health and the Weight Loss Boost ($149) to enhance fat burning. These supplements help fill nutritional gaps caused by reduced appetite, ensuring your body gets the nutrients it needs to maintain muscle mass and energy throughout your weight loss process.
Conclusion
The evidence is clear: neither GLP-1 medications nor lifestyle changes alone can fully address the challenge of sustainable weight loss. GLP-1 medications, such as semaglutide and tirzepatide, play a role by regulating appetite and slowing digestion. On the other hand, lifestyle adjustments – like resistance training and high-protein diets – help preserve muscle mass, support metabolic health, and reduce the risk of weight regain, which impacts up to two-thirds of individuals who discontinue medication.
Combining these approaches yields even better results. Research involving over 12,000 participants found that integrating lifestyle changes with GLP-1 therapy led to an additional 15.7 pounds of weight loss. Participants also saw improvements in waist circumference, blood pressure, and blood sugar levels. Patrick Welch, PharmD from Intermountain Health, emphasizes this point: "All the clinical trials that showed these medications working also included education on eating and exercise. We see much greater success when lifestyle changes are part of the plan."
"GLP-1 medications can help make those goals achievable, but the real magic happens when patients commit to their health journey." – Anthony Bashall, MD, Cardiologist, Franciscan Physician Network
This philosophy is at the heart of TrimRX’s weight loss program. TrimRX blends medical treatment with behavioral support to optimize results. The program offers personalized GLP-1 therapy alongside unlimited check-ins with medical professionals who tailor your nutrition and exercise plans as you progress. It also includes targeted supplements like GLP-1 Daily Support and Weight Loss Boost to address nutritional needs during the weight loss process.
The key to lasting weight loss lies in a combined approach. Recognizing how GLP-1 medications and lifestyle changes complement each other is essential for achieving and maintaining your goals. Together, they provide a solid foundation for long-term success.
FAQs
What side effects can GLP-1 medications cause?
GLP-1 medications are known for their effectiveness in aiding weight loss, but they can come with some side effects. The more common ones include nausea, vomiting, diarrhea, constipation, and general discomfort in the digestive system. Thankfully, these symptoms are usually mild and often improve as your body gets used to the medication.
However, there are less frequent but more serious risks to be aware of, such as pancreatitis, gallbladder issues, or thyroid-related complications. Additionally, rapid weight loss can sometimes affect skin appearance, leading to sagging or wrinkling, a phenomenon often called "Ozempic face."
If you’re considering GLP-1 medications, it’s crucial to talk openly with your healthcare provider. They can help determine if these treatments are a good fit for you and address any concerns you might have.
How do lifestyle changes work with GLP-1 medications to support weight loss?
Lifestyle changes work hand-in-hand with GLP-1 medications, laying the groundwork for lasting results. Adopting habits like eating a balanced diet, staying active, and managing stress can amplify the weight loss effects of these medications while boosting overall metabolic health.
Making sustainable adjustments to your daily routine helps lower the chances of regaining weight and ensures you get the most out of GLP-1 treatments, leading to steadier and more enduring progress.
Why is combining GLP-1 medications with lifestyle changes important for lasting weight loss?
Combining GLP-1 medications with meaningful lifestyle changes is essential for achieving lasting weight loss. Medications like Semaglutide and Tirzepatide work by curbing appetite and managing hunger hormones, making it easier to reduce calorie intake. But for long-term success, these medications need to be paired with healthy habits like balanced nutrition, regular exercise, and quality sleep.
These lifestyle shifts do more than just maintain weight loss – they enhance overall well-being. From boosting energy levels to improving heart health and mental clarity, the benefits are far-reaching. Together, GLP-1 medications and consistent lifestyle adjustments create a well-rounded strategy for reaching your weight loss goals and fostering a healthier, more vibrant life.
Related Blog Posts

Transforming Lives, One Step at a Time
Keep reading
How to Adjust Weight Loss Goals on GLP-1 Medications
Adjust weight goals on GLP-1 meds by tracking body composition and labs, optimizing protein, activity, sleep, and working with your provider on dosing.
Falsified Mounjaro pens prompt urgent safety advisory
MHRA warns of counterfeit Mounjaro pens (batch D873576); stop use and check batch numbers for infection risk.
Novo Nordisk shares drop as Alzheimer’s hopes for weight-loss drug fade
Novo Nordisk’s semaglutide failed to slow Alzheimer’s in large trials, prompting shares to fall and expert reactions.



