7 Causes of Weight Loss Plateaus on GLP-1 Medications

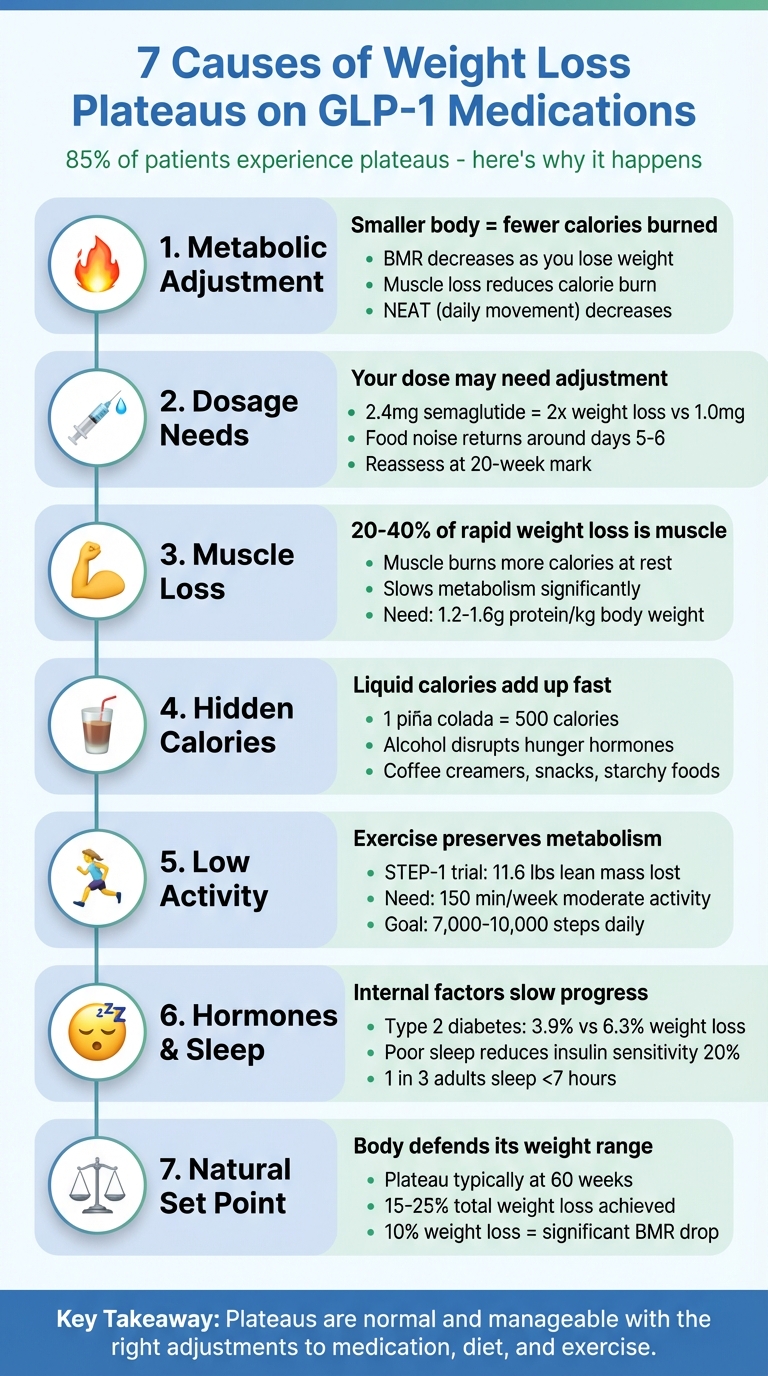
Hitting a weight loss plateau on GLP-1 medications like Semaglutide or Wegovy is common and temporary. Around 85% of people experience plateaus due to metabolic changes, dosage needs, muscle loss, hidden calories, reduced activity, hormonal shifts, or your body’s natural weight "set point." Here’s why it happens and how to overcome it:
- Metabolism slows down as you lose weight. A smaller body burns fewer calories, requiring adjustments to diet and exercise.
- Your GLP-1 dose might need an increase. If hunger returns or progress stalls for weeks, consult your doctor.
- Muscle loss can lower calorie burn. Strength training and higher protein intake help preserve muscle.
- Hidden calories sneak in. Drinks, snacks, and starchy foods can add up – track your intake closely.
- Low physical activity limits progress. Resistance exercises and daily movement boost metabolism.
- Hormones, stress, or sleep issues may interfere. Poor sleep or conditions like PCOS can slow results.
- Your body may reach a natural "set point." Adjust your plan to maintain progress.
Plateaus are normal and manageable. Focus on recalibrating your approach with small, consistent changes. Consult your provider for tailored adjustments to your medication, diet, and exercise plan.
7 Causes of Weight Loss Plateaus on GLP-1 Medications
10 Reasons You Are NOT Losing Weight On GLP-1s
1. Your Metabolism Has Adjusted to Your Lower Weight
When you lose weight, your body’s calorie needs naturally decrease. A smaller body requires less energy to perform basic functions like keeping your heart beating and lungs working. This drop in Basal Metabolic Rate (BMR) means the calorie deficit that helped you shed pounds early in your GLP-1 journey might no longer be enough to keep the weight coming off.
This phenomenon, called adaptive thermogenesis, is your body’s way of adapting to changes. Dr. Daniel A. Nadeau, an expert in obesity medicine, explains:
"The rate of weight loss with Ozempic slows as the months pass, eventually reaching a new equilibrium when calories in (reduced by Ozempic) equal calories burned."
Even though your GLP-1 medication continues to suppress appetite and regulate blood sugar, your body has reached a new balance point. This shift means you’ll need to tweak your diet and activity levels to keep progressing.
But there’s more to it than just weighing less. Losing weight often involves losing some muscle along with fat, and since muscle burns more calories than fat, your daily energy expenditure drops further. Additionally, your NEAT (Non-Exercise Activity Thermogenesis) – the calories burned through everyday movements – also decreases. A lighter body simply uses less energy to move, further reducing how many calories you burn.
Key Metabolic Adjustments to Address Plateaus
| Metabolic Factor | How It Contributes to Plateaus | What to Do About It |
|---|---|---|
| Body Mass | Smaller bodies burn fewer calories at rest | Recalculate daily calorie needs for your current weight |
| Muscle Loss | Less muscle lowers your resting metabolic rate | Incorporate strength training and eat more protein |
| NEAT | A lighter body moves less, burning fewer calories | Track daily steps and aim for 7,000–10,000 |
The solution isn’t to drastically cut calories. Instead, focus on recalculating your caloric needs based on your current weight. Add resistance training 2–3 times a week to preserve or rebuild muscle, and aim to consume 0.6 to 0.75 grams of protein per pound of your goal weight. These changes help maintain your metabolism and keep you on track with your weight loss goals.
2. Your GLP-1 Dose May Need Adjustment
Sometimes, the dose you started with might not be enough to keep the weight loss going. GLP-1 medications work on a dose-dependent basis, meaning higher doses often lead to greater weight loss. For example, clinical trials found that participants taking 2.4 mg of semaglutide lost almost twice as much weight as those on 1.0 mg.
One sign that your dose may need tweaking is the return of "food noise" – those persistent thoughts about food that the medication initially suppressed. If you notice you’re thinking about food more often or feeling hungry around days 5 or 6 after your weekly injection, it could mean your blood levels are dipping too low to stay effective.
"Some people feel the effects immediately and start seeing weight loss, whereas others need to be at higher doses to see results." – Dr. Mir Ali, Medical Director of MemorialCare Surgical Weight Loss Center
Another red flag is reaching the 20-week mark without seeing much progress. If you haven’t experienced meaningful weight loss within the first five months, your current dose might not be sufficient. Additionally, if your weight loss stalls for 3–4 weeks and you’re not experiencing significant side effects, it could indicate your body can handle a higher dose.
Before asking for a dose increase, stick with your current dose for at least four weeks to confirm the plateau is real. Keep track of any side effects weekly – if they’re minimal, discuss a potential dose escalation with your doctor. However, if you’re already on the maximum dose of semaglutide (2.4 mg) and your weight loss has stalled for more than a month, consider talking to your provider about switching to tirzepatide. This dual-agonist medication targets two hormone receptors instead of one, which might help jumpstart progress.
"If a patient is on semaglutide and at maximal dose, then changing to tirzepatide may help since that medication affects two hormone receptor types, as opposed to one." – Dr. Mir Ali
For those on higher doses (2.0 mg per week or more), splitting your injection into two smaller doses – spreading them out over the week – can help maintain steadier blood levels. This method may not only restart progress but also reduce side effects. Adjusting your approach as your body changes is key to keeping your weight loss plan on track.
3. You’re Losing Muscle Along with Fat
When you lose weight quickly with GLP-1 medications, you’re not just shedding fat – you’re losing muscle too. And here’s the kicker: muscle burns calories even when you’re at rest. So, when muscle mass decreases, your metabolism slows down, and that contributes to the dreaded weight loss plateau.
Research suggests that 20%–40% of rapid weight loss can come from lean muscle. This loss prompts your body to conserve energy by burning muscle instead of fat. Dr. Daniel A. Nadeau, an expert in obesity medicine, explains it like this:
"Your metabolism may also slow if you’re losing muscle mass. This is your body’s way of protecting itself from losing too much weight."
The effects of muscle loss are often easy to spot. You might feel weaker, struggle to lift weights you used to handle easily, or notice persistent fatigue. Your muscles may also appear softer and less defined, even though the scale shows a lower number. Dr. Mir Ali, a bariatric surgeon at Orange Coast Medical Center, highlights the importance of exercise and diet in preventing this:
"If you’re not actively exercising – specifically strength training, such as lifting weights – and upping your intake of protein… then this could be a reason for your weight loss plateau."
To keep your metabolism running strong and avoid losing muscle, it’s crucial to prioritize both nutrition and exercise. Aim to eat 1.2 to 1.6 grams of protein per kilogram of body weight daily – for a 150-pound person, that’s about 82 to 109 grams of protein. Include protein-rich foods like eggs, Greek yogurt, fish, lean meats, and beans in every meal. Pair this with resistance training two to three times a week. Even basic bodyweight exercises like squats, push-ups, or planks can signal your body to preserve muscle instead of breaking it down.
4. Hidden Calories and Nutrition Gaps
When you’re on GLP-1 medications, small, often unnoticed dietary habits – like hidden calories and nutritional gaps – can sneak in and stall your progress. One of the biggest culprits? Liquid calories. Drinks like sodas, juices, lattes, and alcohol may seem harmless, but they don’t make you feel full. For instance, just one 8-ounce piña colada contains around 500 calories. Dr. Mir Ali, a bariatric surgeon at Orange Coast Medical Center, explains:
"Consuming a high amount of calories can still lead to weight gain or a plateau, even on these medications. Consider decreasing high-calorie options like sugary foods or simple carbohydrates as an initial step."
Even with medication, excess calories can hold you back. Cutting back on sugary foods and simple carbs is a good place to start.
Alcohol, in particular, requires extra attention. Not only does it add empty calories, but it also disrupts hunger hormones like ghrelin and leptin, which can counteract the appetite-suppressing effects of your medication. Other sneaky sources of calories include coffee creamers, chips, and frequent small snacks that can add up quickly. Even starchy vegetables like potatoes and corn or high-sugar fruits such as ripe bananas and mangoes can contribute more calories than you’d expect.
But it’s not just about hidden calories – nutritional gaps can also slow your progress. When appetite decreases significantly, it’s easy to unintentionally skip meals or fall short on protein intake. To maintain muscle mass, aim for at least 60 grams of protein daily. Samantha Snashall, a registered dietitian at Ohio State Wexner Medical Center, warns:
"Be careful if the volume on the food noise goes down so low while on a GLP-1 that you forget to eat three meals and a couple of snacks a day. If that happens, you can risk becoming malnourished."
Skipping meals due to reduced hunger can lead to malnutrition, which is another obstacle to avoid.
To tackle both hidden calories and nutritional gaps, start by tracking everything you eat and drink for a full week, including those "just a bite" moments. Swap sugary drinks for water, include protein with every meal, and focus on fiber-rich, non-starchy vegetables like broccoli, tomatoes, and leafy greens. These straightforward changes can help you uncover calorie creep and ensure your body is getting the nutrients it needs.
sbb-itb-e2779c3
5. Not Enough Physical Activity
GLP-1 medications help curb appetite, but they don’t increase calorie burn or build muscle. Here’s the thing: a smaller body naturally requires fewer calories to function. Without exercise to keep your metabolism active, the gap between calories consumed and burned shrinks, which can slow down or stall weight loss. This is why staying physically active is so important – it helps counterbalance these metabolic changes.
Losing muscle adds another layer to the challenge. Muscle burns more calories than fat, even at rest, so losing it slows your metabolism even further. For example, in the STEP-1 clinical trial, participants taking semaglutide lost an average of 11.6 pounds of lean body mass compared to just 4 pounds in the placebo group. That’s a big metabolic setback. Dr. Mir Ali, a bariatric surgeon at Orange Coast Medical Center, highlights this issue:
"Without a complementary approach involving nutrition changes and physical activity, your weight loss may stall."
To push past a plateau, resistance training is key. Incorporate resistance exercises 2–3 times a week to help maintain muscle and rev up your metabolism. Studies suggest that supervised resistance training – performed at least 65% of your one-rep max over 12 to 24 weeks – can reduce muscle loss by more than 90% during calorie restriction. Pair this with 150 minutes of moderate aerobic activity per week to increase calorie burn.
Don’t forget about daily movement. Activities like taking the stairs, walking while on calls, or even standing while working – collectively known as non-exercise activity thermogenesis (NEAT) – can make a big difference. Aim for 7,000 to 10,000 steps a day to burn extra calories without making you hungrier. And if you’ve been sticking to the same workout routine for months, your body may have adapted and become more efficient, burning fewer calories. Shake things up by trying new exercises, increasing intensity, or tweaking the duration to give your metabolism a fresh challenge.
6. Hormones, Stress, Sleep, or Medical Conditions
Sometimes, internal factors like hormonal shifts or medical conditions can derail your weight loss efforts, even when you’re eating right and staying active. Conditions such as hypothyroidism, polycystic ovary syndrome (PCOS), or severe insulin resistance can significantly slow progress. The BodySpec Team points out that untreated hypothyroidism, PCOS, or severe insulin resistance can cut expected weight loss in half.
Take the clinical trials for Wegovy as an example: participants with type 2 diabetes lost an average of 3.9% of their body weight within three months, compared to 6.3% in those without diabetes. That 2.4% gap is due to metabolic resistance. For individuals with PCOS or insulin resistance, the body may not respond as effectively to GLP-1 medications, leading to less noticeable results. On top of that, everyday factors like stress and poor sleep can further complicate weight loss.
Stress and lack of sleep create their own challenges. According to Cleveland Clinic, stress hormones can increase cravings for sugary or fatty foods while also slowing your metabolism, making it harder to burn calories. Poor sleep compounds the issue – just four nights of sleeping five hours can reduce insulin sensitivity by about 20%. Unfortunately, one in three adults in the U.S. gets less than seven hours of sleep per night, which can directly undermine the benefits of GLP-1 medications.
If you’ve hit a weight-loss plateau for over a month, it’s time to dig deeper into your metabolic health. Talk to your healthcare provider about getting a full metabolic panel, which should include tests like TSH, free T4, fasting insulin, HbA1c, and an androgen profile. These tests can help identify issues like thyroid problems, insulin resistance, or PCOS. Keep in mind that some medications for these conditions – such as insulin, sulfonylureas, or certain beta-blockers – can contribute to weight gain. Your provider can adjust your GLP-1 treatment while addressing these underlying conditions.
Don’t overlook the importance of good sleep and managing stress. Aim for 7–9 hours of quality sleep by sticking to a regular bedtime, avoiding screens an hour before bed, and keeping your room cool, dark, and quiet. To reduce stress, try techniques like progressive muscle relaxation, guided visualization, or deep breathing exercises to lower cortisol levels. These small but impactful steps can help get your weight loss back on track, even when your biology seems to be working against you.
7. You’ve Reached a Natural Set Point
Your body has a built-in "set point" – a weight range it naturally tries to maintain. When you lose weight, your body responds by increasing ghrelin (the hormone that makes you feel hungry) and decreasing leptin (the hormone that signals fullness). At the same time, it slows down your metabolism to conserve energy. This isn’t a sign that your medication has stopped working; it’s simply your body striving to maintain balance, or homeostasis. This natural response is one of the reasons plateaus often occur during long-term GLP-1 treatment.
"No one loses 100% of their weight. Just like when you give medicine for blood pressure, the pressure falls but not to zero. It stabilizes at some point." – Craig Primack, MD, Founder, Scottsdale Weight Loss Center
Clinical trials reveal that users of Wegovy typically hit a plateau around 60 weeks, achieving a weight loss of 15%–25% of their starting weight. For every 10% reduction in body weight, your resting metabolic rate drops significantly. This means the gap between the calories you eat and the calories you burn narrows, eventually leading to a balance.
Interestingly, as these metabolic changes occur, you might notice improvements in your body shape even if the scale doesn’t budge. This could be a sign of body recomposition – where fat is replaced with muscle. To track progress, focus on non-scale victories like a smaller waistline or how your clothes fit. Don’t forget to adjust your caloric intake after every 5–10 pounds lost, as the calorie deficit needed at your starting weight may no longer apply.
If your weight stays steady for more than four weeks despite sticking to your plan, it might be time to check in with your healthcare provider. They can help fine-tune your strategy, whether that means adjusting your medication dosage or tweaking your exercise routine. To keep your metabolism active and preserve muscle, aim for resistance training 2–3 times a week and consume 0.6 to 0.75 grams of protein per pound of your target body weight. These habits can make a big difference as your body works to find its new balance.
Conclusion
Hitting a weight loss plateau while on GLP-1 medications is more common than you might think. In fact, around 85% of patients encounter this phase, which stems from a mix of factors like metabolic shifts, dosage challenges, muscle loss, hidden calories, reduced activity, hormonal changes, and natural body weight set points. Rather than seeing plateaus as setbacks, it’s important to view them as a normal part of the process.
The good news? You can work through these plateaus by tackling the root causes. Start by consulting your healthcare provider if progress stalls. They can help adjust your medication dosage, order tests to check for thyroid or metabolic concerns, and fine-tune your diet and exercise plan. Keep in mind that about 14% of people taking semaglutide may lose less than 5% of their body weight after 68 weeks, so for some, exploring alternatives like tirzepatide – designed to target multiple hormone receptors – might be necessary.
"Weight management is a long game. With the right guidance and consistency, small steps can lead to big, lasting change." – Wesley McWhorter, DrPH, Academy of Nutrition and Dietetics
Navigating these challenges is easier with a personalized approach. Programs like TrimRX offer tailored consultations, medication adjustments, and ongoing support to help you break through plateaus. With the right tools and guidance, sustainable weight loss becomes achievable, and you’re never left to figure it out on your own.
FAQs
What can I do to break through a weight loss plateau while on GLP-1 medications?
Hitting a weight loss plateau while taking GLP-1 medications like semaglutide or Wegovy can feel discouraging, but tweaking your diet and activity levels might get things moving again. Start by reassessing your calorie intake – weight loss often slows your metabolism, meaning you may need to slightly lower your calorie target. Keep a food journal for a week to track what you’re eating, and prioritize nutrient-rich choices like lean protein (aim for about 30g per meal) and high-fiber vegetables. Cut back on liquid calories from sugary drinks, alcohol, or calorie-heavy coffee extras, and trade processed snacks for whole, less-processed foods.
On the exercise front, a mix of strength training and cardio can help rev up your metabolism and maintain muscle. Try resistance training 2–3 times per week using dumbbells, resistance bands, or body weight exercises. Pair this with at least 150 minutes of moderate-intensity cardio, such as brisk walking or cycling, each week. Small daily habits, like taking the stairs or going for short walks, can also add up. If you’re still stuck, consider gradually increasing the intensity or duration of your workouts – but always check with your healthcare provider before making major changes. By fine-tuning your diet and exercise routine, you can break through the plateau and keep moving toward your weight loss goals.
How can I tell if my GLP-1 medication dosage needs to be adjusted?
If you’ve been using a GLP-1 medication and notice that your weight loss has plateaued for several weeks, it could indicate that your current dose isn’t sufficient. This often happens during the titration phase, where doses are gradually adjusted to find the right balance for effective results.
Before making any changes, it’s essential to talk to your healthcare provider. They can assess your progress and help decide if an increased dosage is the right step for you.
Can hormonal changes or medical conditions cause weight loss plateaus with GLP-1 medications?
Hormonal imbalances and specific medical conditions can sometimes lead to weight loss plateaus when using GLP-1 medications like Semaglutide or Wegovy. For example, conditions such as thyroid disorders, polycystic ovary syndrome (PCOS), and insulin resistance can affect how well these medications manage appetite and metabolism.
If you hit a plateau, reaching out to your healthcare provider is essential. They can investigate potential underlying causes and make adjustments to your treatment plan to help you stay on track with your weight loss goals.
Related Blog Posts

Transforming Lives, One Step at a Time
Keep reading
How to Adjust Weight Loss Goals on GLP-1 Medications
Adjust weight goals on GLP-1 meds by tracking body composition and labs, optimizing protein, activity, sleep, and working with your provider on dosing.
Falsified Mounjaro pens prompt urgent safety advisory
MHRA warns of counterfeit Mounjaro pens (batch D873576); stop use and check batch numbers for infection risk.
Novo Nordisk shares drop as Alzheimer’s hopes for weight-loss drug fade
Novo Nordisk’s semaglutide failed to slow Alzheimer’s in large trials, prompting shares to fall and expert reactions.



