GLP-1 Injection Site Reactions: Causes and Fixes

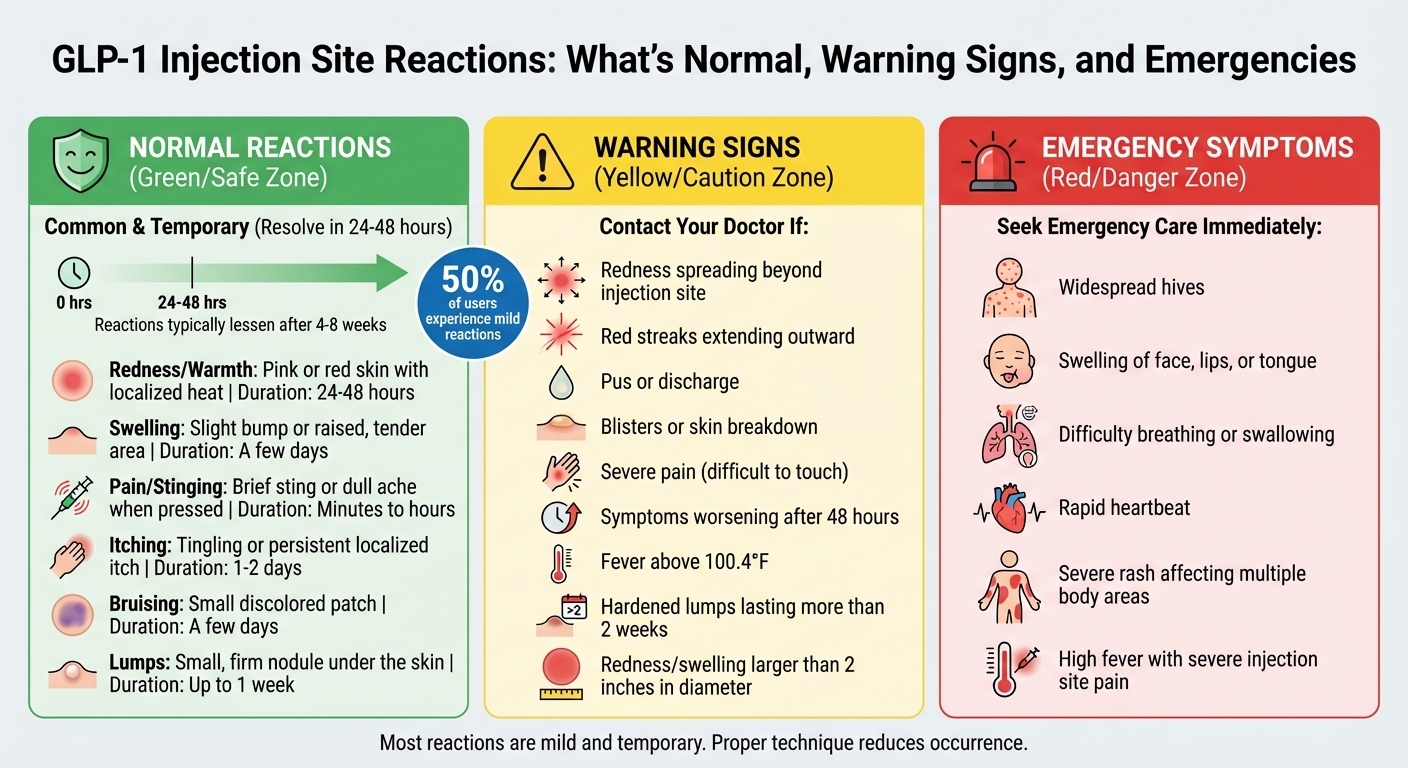
GLP-1 medications like Semaglutide (Ozempic, Wegovy) and Tirzepatide (Mounjaro, Zepbound) are effective for weight loss, but about 50% of users experience mild injection site reactions. These reactions – such as redness, swelling, itching, or small bruises – are usually temporary and clear up within 24 to 48 hours. Proper injection techniques, site rotation, and skin preparation can minimize discomfort. Serious symptoms like spreading redness, pus, or fever require medical attention.
Key Takeaways:
- Common Reactions: Redness, swelling, itching, bruises, or lumps (lasting up to a week).
- Prevention Tips: Rotate injection sites, let alcohol dry before injecting, and allow refrigerated pens to reach room temperature.
- When to See a Doctor: Symptoms worsen after 48 hours, include pus, or are accompanied by fever.
- Emergency Signs: Trouble breathing, facial swelling, or widespread hives.
By following proper preparation and technique, most users can manage and reduce these reactions effectively.
How to avoid injection site reactions with Mounjaro or Ozempic & when are they serious?
Common GLP-1 Injection Site Reactions
GLP-1 Injection Site Reactions: Types, Symptoms, Duration and When to Seek Help
Normal Reactions
When starting GLP-1 medications, mild and temporary reactions at the injection site are fairly common. These usually resolve on their own within 24 to 48 hours. Dr. Ameen Masoodi, a Family Medicine Physician, explains:
"Injection site reactions are common, but they are usually mild and diminish as you become used to the medication."
Here’s what you might notice: redness or pink skin that feels warm to the touch, mild swelling forming a small raised bump, a brief sting or dull ache during or right after the injection, itching, small bruises from hitting tiny blood vessels, or firm lumps that can last up to a week. Most of these effects tend to lessen in frequency and intensity after your body adjusts to the medication, which typically happens within 4 to 8 weeks.
| Reaction Type | Description | Duration |
|---|---|---|
| Redness/Warmth | Pink or red skin with localized heat | 24–48 hours |
| Swelling | Slight bump or raised, tender area | A few days |
| Pain/Stinging | Brief sting or dull ache when pressed | Minutes to hours |
| Itching | Tingling or persistent localized itch | 1–2 days |
| Bruising | Small discolored patch | A few days |
| Lumps | Small, firm nodule under the skin | Up to 1 week |
These minor reactions are typical, but it’s important to recognize when something more serious might be happening. Let’s look at signs that call for medical attention.
Warning Signs That Need Medical Attention
While most injection site reactions are harmless, some symptoms can indicate a problem. Dr. Tracy Norfleet, MD, FACP, notes:
"Injection site reactions may get worse over the first 24 hours, and should improve thereafter. If your symptoms just keep getting worse, something else could be going on."
Contact your doctor if you notice redness spreading beyond the injection site, red streaks extending outward, pus or discharge, blisters or skin breakdown, or severe pain that makes it difficult to touch the area. Also, watch for symptoms that worsen after 48 hours or if a fever above 100.4°F develops.
In rare cases, a serious allergic reaction may occur. Seek emergency care immediately if you experience widespread hives, swelling of the face, lips, or tongue, difficulty breathing or swallowing, or a rapid heartbeat. These symptoms could be life-threatening and need immediate attention.
What Causes GLP-1 Injection Site Reactions
Understanding the reasons behind injection site reactions can help reduce their occurrence. These reactions often stem from three main factors: the medication itself, how you prepare your skin, and your injection technique.
Medication and Formulation Factors
The properties of the medication play a big role in how your skin reacts. For instance, injecting medication straight from the refrigerator can irritate tissues, causing more pain and stinging. Some formulations, like semaglutide, which is 94% similar to the natural GLP-1 hormone, can also trigger reactions.
Another common issue involves residual alcohol left on the skin. If the alcohol from the swab hasn’t fully dried before injecting, it can be carried under the skin, causing a burning sensation. Injection site reactions are relatively common, affecting anywhere from 0.5% to 40% of users. For example, tirzepatide trials reported that up to 10% of participants experienced itching or redness.
Beyond the medication itself, factors like your skin’s condition and how you inject can also influence the severity of reactions.
Skin Sensitivity and Preparation Problems
Preparing your skin properly is key to minimizing irritation. Rushing through preparation or not letting the alcohol swab dry completely can lead to moisture being pushed into the skin with the needle. This often results in stinging and redness that can linger for days.
External factors, like friction from clothing rubbing against the injection site, can make irritation worse. Injecting into areas with scars, bruises, moles, or rashes increases the chances of severe reactions and may even affect how well the medication is absorbed. In fact, studies show that up to 50% of people using GLP-1 injectables like Ozempic report some form of reaction, many of which are tied to avoidable preparation errors.
Injection Technique and Site Rotation Mistakes
Improper technique is another major contributor to injection site issues. Reusing needles can lead to infections, tissue damage, and bruising by harming small blood vessels. Additionally, failing to rotate injection sites can cause lipodystrophy – a condition where fatty tissue builds up in certain areas, creating hard lumps or dents that can interfere with medication absorption.
The angle and depth of the injection also matter. GLP-1 medications are designed to be injected into fatty tissue just beneath the skin. Injecting too deeply into muscle or too shallowly into the dermis can result in more pain and inconsistent medication absorption.
As Yuval Ramot from the Department of Dermatology at Hadassah Medical Center notes:
"Almost all local reactions to subcutaneously administered biological agents can be prevented by changing the injection techniques, patient education, and training."
While most redness and warmth from injections resolve within 24 to 48 hours, mistakes in technique can prolong these symptoms. Proper education and careful practices are essential to avoid unnecessary discomfort.
How to Fix GLP-1 Injection Site Reactions
Once you’ve identified the causes, the good news is that most injection site reactions can be managed at home with simple remedies. Let’s dive into how to address some of the most common issues.
Treating Redness and Swelling
If you notice redness or swelling after your injection, applying a cold compress or an ice pack wrapped in a towel for 10 to 20 minutes can help calm the inflammation and speed up recovery. However, if the swollen area grows larger than 2 inches in diameter or doesn’t improve after two days, it’s time to reach out to your doctor.
For soreness, over-the-counter pain relievers like acetaminophen (Tylenol) or ibuprofen (Advil) can provide relief. A 1% hydrocortisone cream can also soothe irritated skin. Wearing loose clothing can prevent further irritation, and don’t forget to rotate your injection sites. Giving each area time to heal is key to avoiding repeated irritation.
Next, let’s tackle itching and skin irritation.
Relieving Itching and Skin Irritation
Itching is a common reaction, but it’s manageable. Oral antihistamines like cetirizine (Zyrtec), loratadine (Claritin), or diphenhydramine (Benadryl) can help reduce the histamine response that triggers itching. For localized relief, you can try calamine lotion or a cold compress.
Avoid scratching the affected area – it can worsen the redness and increase the risk of infection. If alcohol swabs irritate your skin, consider cleaning the area with mild soap and water instead. Just make sure the skin is completely dry before injecting. As Dr. Andrew J. Shapiro, Medical Director at Wellington Regional Medical Center, explains:
"It is usually temporary and goes away after a few minutes."
If pain or burning persists, there are adjustments you can make to your injection routine.
Reducing Pain, Burning, and Stinging
One simple trick to reduce stinging is to let your refrigerated pen sit at room temperature for 15 to 30 minutes before injecting. This can make a big difference. Also, be sure to let any alcohol used to clean the skin fully evaporate before injecting – it can help minimize irritation.
When injecting, go slowly and steadily, keeping the needle still while it’s in your skin. Always use a fresh, sterile needle for each dose. Interestingly, in clinical trials for 2.4 mg semaglutide, only 0.2% of 407 participants reported a burning sensation, which highlights the importance of proper injection technique.
Preventing Bruising and Lumps
To avoid bruising and lumps, careful site selection and technique are crucial. Check your injection site beforehand and steer clear of areas with visible blood vessels. After injecting, gently press the area with a clean cotton ball or gauze for about 30 seconds – but don’t rub, as this can lead to bruising.
Rotating your injection sites – between the abdomen, thighs, and upper arms – can also prevent lipodystrophy, a condition where fatty tissue builds up and forms hard lumps that may interfere with how your medication is absorbed.
Most small bruises will fade within a week. However, if you notice lumps that persist beyond two weeks or seem to grow, it’s important to consult your healthcare provider for further evaluation.
sbb-itb-e2779c3
When to Contact Your Doctor or Seek Emergency Care
Most injection site reactions are mild and resolve on their own, but knowing when to seek medical attention is essential to avoid complications. Recognizing the signs that warrant professional help can make all the difference.
Contact Your Doctor for These Symptoms
If your symptoms persist or worsen beyond 48 hours, it’s time to reach out to your doctor. Dr. Tracy Norfleet, MD, FACP, advises:
"Injection site may be infected if you notice redness, warmth, or tenderness or swelling in the area, and it keeps getting worse or lasts more than 1 to 2 days."
Here are specific signs that should prompt you to consult your doctor:
- Pus or discharge coming from the injection site
- Warmth spreading beyond the immediate area
- Red streaking extending outward from the injection site
- Redness or swelling larger than 2 inches in diameter
- Hardened lumps that don’t go away, suggesting a possible infection
- Severe pain that disrupts your daily activities
- Reactions lasting more than a week
- Unusual skin discoloration
- Fever accompanied by chills
- New lumps or swelling in your neck, especially with hoarseness or difficulty swallowing
If any of these symptoms appear, don’t delay contacting your healthcare provider.
Go to the Emergency Room for These Symptoms
In some cases, symptoms can signal a severe allergic reaction requiring immediate attention. If you experience anaphylaxis or other serious reactions, call 911 or head to the nearest emergency room. As noted in Ozempic’s official safety information:
"Stop using Ozempic® and get medical help right away if you have any symptoms of a serious allergic reaction, including swelling of your face, lips, tongue, or throat; problems breathing or swallowing; severe rash or itching; fainting or feeling dizzy; or very rapid heartbeat."
Other situations that require emergency care include:
- Widespread hives affecting multiple areas of your body
- Blisters in sensitive areas like your mouth, eyes, or genitals
- High fever combined with severe pain at the injection site
- Sudden, intense abdominal pain radiating to your back (a potential sign of pancreatitis)
- Swelling of your tongue or throat that makes breathing difficult
Don’t hesitate to act if you notice any of these symptoms – quick action can be lifesaving.
How to Prevent Future Injection Site Reactions
Managing injection site reactions starts with proper medication handling and technique. While mild reactions are common – affecting up to 50% of people – they can often be minimized. Two key strategies to address this are adjusting medications to suit individual needs and perfecting your injection technique.
Customized Dosing and Medication Selection
Everyone’s body reacts differently to medications, so finding the right fit is essential. If you’re dealing with ongoing reactions, talk to your healthcare provider about tweaking your dose or exploring alternative medications. For instance, TrimRX offers weight loss programs tailored to individual needs. Their options include Injectable Semaglutide starting at $199, along with other GLP-1 medications, all under expert supervision. Learn more at TrimRX.
Correct Technique and Ongoing Support
Even the best medication can lead to issues if the injection technique isn’t right. Small mistakes, like reusing the same spot too soon, can result in unnecessary irritation. To prevent this, practice proper site rotation – keep at least a 1-inch gap between injection sites and avoid reusing the exact location for at least 4 weeks. Marker Health emphasizes:
"Injection site rotation isn’t optional nice-to-have advice. It’s essential for preventing tissue damage and maintaining consistent medication absorption."
Additional tips include ensuring the skin is completely dry after using an alcohol swab and avoiding areas with scars, tattoos, moles, or any irritation.
For those needing extra guidance, TrimRX offers unlimited check-ins with their medical team. This ongoing coaching ensures your technique improves over time, reducing the likelihood of reactions. As one patient shared:
"The first month was challenging with itchy spots that lasted about 3 days. Now at month 3, I barely notice any reaction at all." – Real patient experience, Klarity.
If reactions persist for more than 48 hours, document them with photos to share with your healthcare provider. This can help pinpoint the issue and adjust your treatment plan effectively.
Conclusion
Most injection site reactions from GLP-1 medications are mild, short-lived, and tend to fade within 24–48 hours. With consistent treatment, these reactions usually become less frequent after 3–4 weeks. By using proper injection techniques, rotating injection sites systematically, and trying simple home remedies like cold compresses or hydrocortisone cream, you can manage most of the discomfort effectively.
It’s important to differentiate between normal reactions and those that may need medical attention. Mild redness, slight swelling, or brief itching are common and typically harmless. However, if you notice redness spreading beyond 2 inches, signs of infection like pus, fever, or symptoms of a severe allergic reaction – such as trouble breathing – seek medical help immediately.
To minimize reactions, follow best practices: let your medication sit at room temperature for 15–30 minutes before injecting, rotate injection sites (keeping at least 1 inch between spots), and ensure your skin is completely dry after cleaning. These small but crucial steps, combined with personalized guidance, can make a big difference over time.
For ongoing support, TrimRX offers customized GLP-1 programs starting at $199 for Injectable Semaglutide. Their program includes unlimited check-ins with their medical team to help you refine your technique and ensure your treatment plan is tailored to your needs. Visit TrimRX to explore their expert-supervised weight loss solutions.
FAQs
How can I reduce reactions at GLP-1 injection sites?
To reduce the chance of irritation or reactions at GLP-1 injection sites, try these practical tips:
- Start with clean skin: Wash your hands thoroughly with soap and water, then disinfect the injection area using an alcohol pad. Allow the skin to dry completely before proceeding.
- Switch up your sites: Rotate between areas like your abdomen (keeping at least 2 inches away from the belly button), thighs, or upper arms. Avoid using the same spot repeatedly to minimize irritation.
- Master the technique: Insert the needle at the proper angle (usually 90°) and always use a fresh needle. Ensure the needle length matches your medication pen’s requirements.
- Post-injection care: After injecting, press a clean cotton ball gently on the site. If the area feels irritated, a cool compress can help ease redness or itching.
- Skip sensitive spots: Avoid injecting into areas with broken, irritated, tattooed, or scarred skin. Tight clothing over the site is also best avoided.
It’s common to experience mild redness, warmth, or itching that subsides within 24–48 hours. However, if you notice severe swelling, redness extending beyond 2 inches, fever, or trouble breathing, reach out to a healthcare provider right away. For those following a TrimRX weight-loss program, these steps can help you use your prescribed GLP-1 medication more comfortably and effectively.
What should I do if my injection site reaction is getting worse?
If the reaction at your injection site seems to be getting worse, don’t wait to act. It’s essential to rule out possible infection or an allergic response. Be on the lookout for serious symptoms, including redness that spreads beyond 2 inches, increasing swelling, intense pain, fever, chills, or trouble breathing. If any of these occur, seek medical care right away.
To help your healthcare provider, document the reaction. Take a photo, note when it began, and track how it changes over time. Reach out to your healthcare provider as soon as possible. If you’re part of a TrimRX program, contact your care team for tailored advice. Until then, avoid injecting into the irritated area – switch to a different site. A warm compress or an over-the-counter pain reliever (if safe for you) might ease the discomfort.
Your provider may suggest treatments like a topical antibiotic, an antihistamine, or changes to your injection technique or medication. Acting on their guidance quickly can help you avoid complications and make future injections more manageable.
How can I prevent bruising and lumps from GLP-1 injections?
To reduce bruising and avoid lumps (lipohypertrophy) from GLP-1 injections, following a few straightforward techniques can make a noticeable difference. Bruising occurs when small blood vessels are disrupted, while repeatedly injecting in the same area can lead to thickened fatty tissue forming lumps. Thankfully, both issues can be avoided with the right approach.
Helpful tips: Rotate your injection sites regularly – move at least 2 inches away from your last injection spot. Steer clear of areas that are red, swollen, or irritated. Use proper needle technique by pinching the skin, inserting the needle at a 90° angle (or 45° if your skin is very thin), and choosing smaller-gauge needles for less discomfort. Always clean the injection site with an alcohol swab and let it air dry before injecting. After the injection, apply gentle pressure with a cotton ball but avoid rubbing the area.
These practices not only protect your skin but also help ensure the medication is absorbed as intended. If you’re part of a TrimRX program, you’ll also benefit from personalized support and guidance on injection techniques tailored to your needs.
Related Blog Posts

Transforming Lives, One Step at a Time
Keep reading
How to Adjust Weight Loss Goals on GLP-1 Medications
Adjust weight goals on GLP-1 meds by tracking body composition and labs, optimizing protein, activity, sleep, and working with your provider on dosing.
Falsified Mounjaro pens prompt urgent safety advisory
MHRA warns of counterfeit Mounjaro pens (batch D873576); stop use and check batch numbers for infection risk.
Novo Nordisk shares drop as Alzheimer’s hopes for weight-loss drug fade
Novo Nordisk’s semaglutide failed to slow Alzheimer’s in large trials, prompting shares to fall and expert reactions.



