Cardiovascular Risks of GLP-1 Medications

GLP-1 receptor agonists, like semaglutide, liraglutide, dulaglutide, and tirzepatide, are widely used for managing type 2 diabetes and obesity. These medications not only help with weight loss and blood sugar control but also reduce cardiovascular risks, including heart attacks and strokes, especially in high-risk patients. However, they come with potential side effects such as a slight increase in resting heart rate, risks for heart failure in certain groups, and complications for individuals with diabetic retinopathy. Careful patient monitoring and tailored dosing are essential to balance benefits and risks effectively.
Key Takeaways:
- Benefits: Lower risk of major cardiovascular events (up to 40% in some studies), improved blood sugar, and weight loss.
- Risks: Increased heart rate, potential worsening of heart failure with reduced ejection fraction, and rare complications like hypoglycemia or retinopathy.
- Monitoring Tips: Regular heart rate, blood pressure, and eye exams are crucial. Gradual dose increases can minimize side effects.
- Drug Interactions: Combining GLP-1 medications with SGLT2 inhibitors may enhance heart and kidney health, but caution is needed with insulin or sulfonylureas.
These therapies offer promising outcomes for heart health but require personalized care and consistent follow-ups to ensure safety.
Cardiovascular Benefits of GLP-1 Medications
Results from Cardiovascular Outcome Trials
Clinical trials have shown that GLP-1 receptor agonists not only improve blood sugar levels but also provide protection for the heart. In the SOUL trial, published in March 2025 in the New England Journal of Medicine, researchers studied 9,650 participants aged 50 and older with type 2 diabetes and either cardiovascular or kidney disease. These participants were randomly assigned to receive 14 mg of oral semaglutide daily. The study, led by Dr. Darren K. McGuire, found that oral semaglutide reduced major adverse cardiovascular events (MACE) to 3.1 events per 100 person-years, compared to 3.7 events in the placebo group – a 14% reduction (HR 0.86) over a median follow-up of 49.5 months.
The PIONEER 6 trial further supported these findings. Among 3,183 high-risk patients with type 2 diabetes, oral semaglutide cut cardiovascular deaths by 51% (HR 0.49) and reduced all-cause mortality by 49% (HR 0.51) over a median follow-up of 15.9 months. Similarly, the SUSTAIN-6 trial revealed that subcutaneous semaglutide reduced MACE by 26% in patients with type 2 diabetes at high risk for heart problems.
Other GLP-1 receptor agonists have shown comparable results. The LEADER trial with liraglutide reported a reduction in MACE (HR 0.87), while the REWIND trial with dulaglutide demonstrated an HR of 0.88. A systematic review pooling data from 27,617 patients found that semaglutide use lowered MACE risk by 19% overall (RR 0.81).
Benefits in High-Risk Patient Groups
GLP-1 receptor agonists also show heart-protective effects in other vulnerable groups. The SUMMIT trial, conducted by Eli Lilly and published in November 2024, focused on 731 patients with both heart failure (ejection fraction ≥50%) and obesity. Led by Dr. Milton Packer, the study found that tirzepatide reduced the combined risk of cardiovascular death or worsening heart failure by 38% (HR 0.62) over a median of 104 weeks. The risk of worsening heart failure events alone dropped by 46% (HR 0.54).
Additional studies highlight benefits for older adults and those with chronic kidney disease. In one observational study involving adults with type 2 diabetes and ischemic heart disease, tirzepatide was linked to a 40% lower risk of a composite outcome, including heart attack, stroke, and all-cause mortality (HR 0.60). High-risk diabetic patients with a history of heart attack also saw a 36% reduction in atrial arrhythmias and a 38% drop in atrial fibrillation when treated with semaglutide. These findings open doors for further research into managing potential drug interactions and addressing cardiovascular side effects.
Cardiovascular Risks and Precautions
Uncommon Cardiovascular Risks
While GLP-1 agonists are known for their heart-protective benefits, they come with certain cardiovascular risks that shouldn’t be overlooked. One of the most consistent findings in clinical trials is a slight increase in resting heart rate, typically between 2 and 4 beats per minute. For example, the PIONEER 6 trial, conducted from January to August 2017, reported an average increase of 4 beats per minute in patients taking oral semaglutide. While this change may seem small, it can be significant for patients who are already at risk.
Particular caution is needed for patients with heart failure with reduced ejection fraction (HFrEF). The LIVE trial highlighted an uptick in serious cardiac events, such as ventricular tachycardia and worsening heart failure, in this group. As the Cardiology and Therapy Journal explains:
Increased heart rates have been linked to poor outcomes in HF and may help explain the findings from the LIVE trial.
Other risks include an increased likelihood of hypotension and syncope. In the PIONEER 6 trial, hypoglycemia was reported in 1.4% of patients using oral semaglutide compared to 0.8% in the placebo group. This risk becomes even more pronounced when GLP-1 medications are paired with insulin or sulfonylureas. Additionally, patients with diabetic retinopathy should proceed with caution, particularly when using subcutaneous semaglutide, as some trials have reported a higher incidence of retinopathy-related complications. These findings underscore the importance of careful monitoring to address these potential risks.
The Role of Patient Monitoring
To address these cardiovascular risks, close and consistent monitoring is essential. The potential for increased heart rate and hypotension highlights the need for regular oversight to ensure patient safety. Healthcare providers should assess heart rate and blood pressure both at the start of treatment and throughout its course, especially for patients with arrhythmias or heart failure.
For patients with a history of diabetic retinopathy, regular eye exams are a must when beginning GLP-1 therapy. Yosra Turkistani from Umm Al-Qura University advises:
Subcutaneous semaglutide should be used cautiously in patients with pre-existing diabetic retinopathy.
Starting treatment at a low dose and gradually increasing it can help reduce side effects while allowing healthcare providers to monitor cardiovascular tolerance. This careful approach, paired with frequent follow-ups, enables clinicians to track changes in heart rate, glycemic control, and any emerging complications before they become serious concerns.
Drug Interactions and Cardiovascular Effects
Common Drug Interactions with GLP-1 Medications
When using GLP-1 receptor agonists to improve cardiovascular health, it’s crucial to understand how these medications interact with others. These drugs are often paired with other treatments, and knowing how they work together is key to ensuring cardiovascular safety. For example, medications like ACE inhibitors, ARBs, and beta-blockers generally do not interfere with the cardiovascular benefits of GLP-1 therapies. Clinical trials have shown that these benefits remain consistent even when these drugs are used together.
One particularly exciting combination is GLP-1 medications with SGLT2 inhibitors. Research from global trials shows that combining these two therapies offers independent and additive cardiovascular benefits, making this pairing a standout option for many patients. These findings are shaping treatment guidelines, encouraging the use of this combination to maximize patient outcomes.
That said, there are some combinations that require extra care. Insulin and sulfonylureas, when used alongside GLP-1 medications, can increase the risk of hypoglycemia. While GLP-1 therapies alone have a low risk of causing low blood sugar, adding insulin or sulfonylureas to the mix calls for careful dosage adjustments and close monitoring.
Guidelines for Safe Medication Use
Based on these findings, current medical guidelines include specific recommendations to ensure safe use. Both the American Diabetes Association (ADA) and the European Society of Cardiology (ESC) now advocate for GLP-1 receptor agonists in patients with atherosclerotic cardiovascular disease, regardless of their initial HbA1c levels. The ADA highlights the benefits of combining GLP-1 receptor agonists with SGLT2 inhibitors, stating:
Combined use [of GLP-1 RAs and SGLT2 inhibitors] may be considered for additive cardio-kidney protection.
Timing is also critical when it comes to surgical procedures. For patients on daily GLP-1 formulations, the medication should be paused on the day of an elective surgery. Meanwhile, weekly formulations should be stopped a full week beforehand to reduce risks tied to delayed gastric emptying. Additionally, patients with heart failure – especially those with reduced ejection fraction – should be monitored closely for increases in heart rate when starting GLP-1 therapies.
The trend of combining therapies continues to gain momentum, with growing support for pairing GLP-1 receptor agonists and SGLT2 inhibitors. This approach is proving effective at delivering both cardiovascular and kidney benefits, offering a powerful strategy for improving patient outcomes.
sbb-itb-e2779c3
A meta-analysis of the efficacy of GLP-1 receptor agonists in the prevention of stroke
Risk Management and Monitoring Strategies
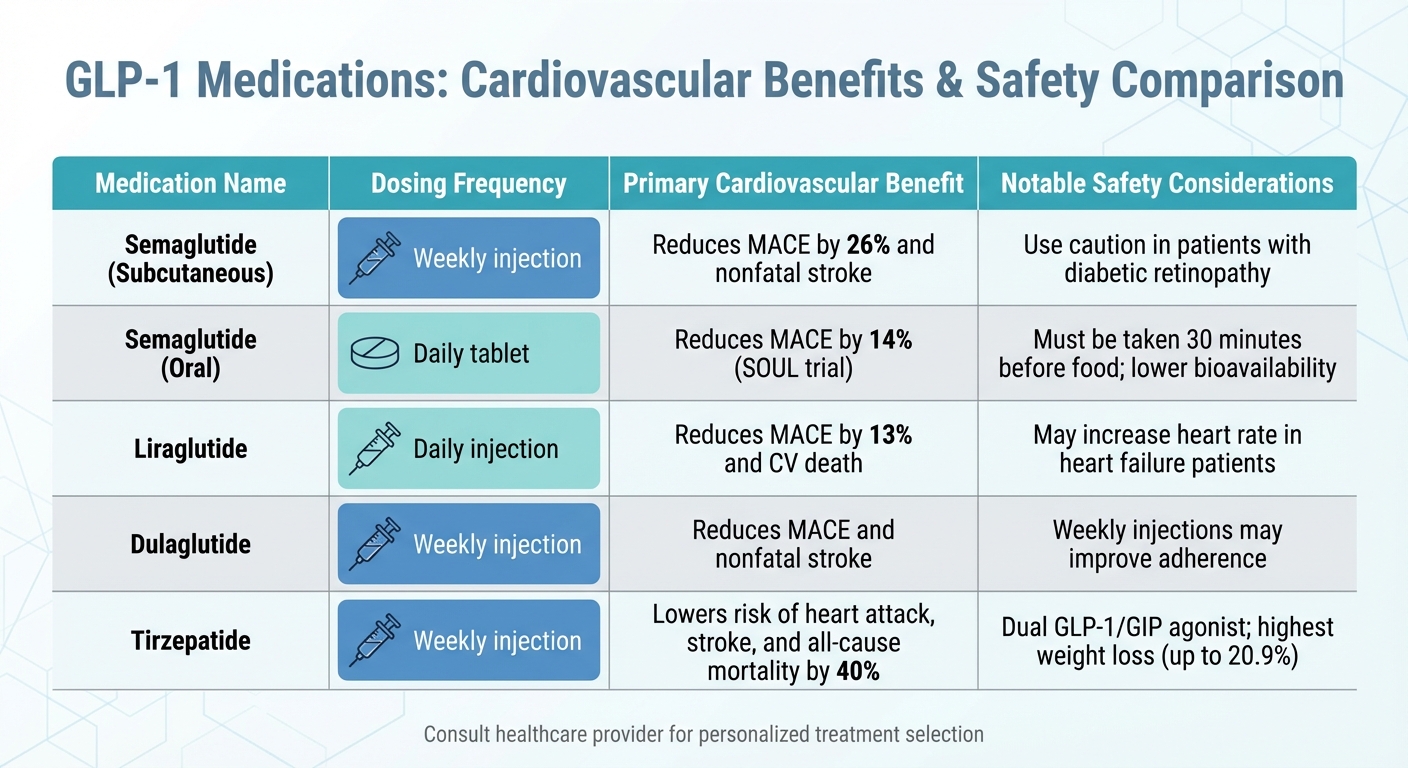
GLP-1 Medications Comparison: Cardiovascular Benefits and Safety Profiles
Patient Selection and Initial Assessments
Before starting GLP-1 therapy, it’s essential to perform a detailed cardiovascular screening. The best candidates are usually individuals aged 55 or older who have at least two cardiovascular risk factors – such as obesity, high blood pressure, smoking, high cholesterol, or protein in the urine – or those already diagnosed with atherosclerotic cardiovascular disease. This initial evaluation should also include kidney function tests, as these medications are generally avoided in patients with severe kidney dysfunction.
It’s equally important to check for contraindications, including a personal or family history of medullary thyroid cancer, MEN 2A/2B, or pancreatitis. For patients on warfarin, monitoring the International Normalized Ratio (INR) is advised due to the potential impact of delayed gastric emptying.
Once eligibility is confirmed and contraindications are ruled out, treatment can begin with careful dosing and ongoing monitoring.
Regular Monitoring and Dose Adjustments
After completing the baseline assessments, therapy should start with a gradual dose escalation. For example, with semaglutide, begin at 0.25 mg weekly, increasing every four weeks. This slow titration helps reduce common gastrointestinal side effects like nausea and vomiting. It’s worth noting that about 10% of patients discontinue GLP-1 therapy due to these side effects, so careful dose adjustments can significantly improve tolerability.
Regular follow-ups are crucial. These check-ins should include monitoring HbA1c levels, blood pressure, lipid profiles, and kidney function (serum creatinine and eGFR), especially during dose increases. For patients using insulin or sulfonylureas, reducing their doses by 25% when starting GLP-1 therapy can help avoid hypoglycemia. Additionally, patients experiencing severe vomiting or diarrhea should be monitored for dehydration and acute kidney injury.
This structured approach not only improves the tolerability of the medication but also enhances cardiovascular outcomes.
Comparison of GLP-1 Medication Types
Different GLP-1 medications vary in their cardiovascular benefits and safety considerations, making it essential to choose the right one for each patient.
| Medication | Frequency | Primary CV Benefit | Notable Safety Profile |
|---|---|---|---|
| Semaglutide (Subcutaneous) | Weekly | Reduces MACE by 26% and nonfatal stroke | Use caution in patients with diabetic retinopathy |
| Semaglutide (Oral) | Daily | Reduces MACE by 14% (SOUL trial) | Must be taken 30 minutes before food; lower bioavailability |
| Liraglutide | Daily | Reduces MACE by 13% and CV death | May increase heart rate in heart failure patients |
| Dulaglutide | Weekly | Reduces MACE and nonfatal stroke | Weekly injections may improve adherence |
| Tirzepatide | Weekly | Lowers risk of heart attack, stroke, and all-cause mortality by 40% | Dual GLP-1/GIP agonist; highest weight loss (up to 20.9%) |
The choice of medication should be tailored to the patient’s specific needs and health profile. For example, when switching between formulations – such as from oral to injectable semaglutide – ensure equivalent dosing. A 14 mg oral dose of semaglutide is roughly comparable to 0.5 mg injectable, though switching may not be suitable for patients on higher doses. Additionally, women planning to conceive should stop GLP-1 medications at least two months before pregnancy.
Conclusion
GLP-1 therapies have shown promise in improving heart health and supporting weight loss, with major trials highlighting their ability to reduce key cardiovascular events across a variety of patient groups. These medications are increasingly recognized for their role in lowering the risk of adverse outcomes, making them a valuable option in managing cardiovascular health.
However, like all treatments, GLP-1 therapies come with potential drawbacks. Common side effects include gastrointestinal issues, which lead to about 10% of patients discontinuing use, as well as risks like hypotension, pancreatitis, and the progression of diabetic retinopathy. Research from Umm Al-Qura University emphasizes the cardioprotective benefits of GLP-1 receptor agonists, along with their low risk of causing hypoglycemia, underscoring their value in a well-rounded approach to reducing cardiovascular disease. Achieving the best results depends on careful patient selection, gradual dose adjustments, and consistent monitoring.
Partnering with your healthcare provider is key to crafting a treatment plan that maximizes cardiovascular benefits while managing potential risks. This process often involves screening for contraindications, adjusting other medications like insulin, and incorporating lifestyle changes – such as resistance training – to maintain muscle mass during weight loss.
For those exploring GLP-1 therapy, TrimRX offers personalized programs, including tailored consultations, prescriptions, and ongoing support to help ensure safe and effective results.
FAQs
What cardiovascular benefits do GLP-1 medications offer for patients at high risk?
GLP-1 receptor agonists offer notable benefits for individuals at high risk of cardiovascular issues. These medications are effective in reducing the chances of major adverse cardiovascular events, such as cardiovascular death, non-fatal heart attacks, and strokes. Beyond that, they help improve key health markers like blood pressure, cholesterol levels, and body weight. They’ve also been shown to decrease the risk of hospitalizations due to heart failure and reduce the occurrence of irregular heart rhythms.
By targeting several risk factors at once, GLP-1 medications not only protect heart health but also contribute to better overall health, making them a valuable treatment option for those with elevated cardiovascular risks.
Can GLP-1 medications be taken with insulin or other diabetes treatments?
GLP-1 receptor agonists, such as Ozempic®, can be used together with other diabetes medications, including insulin, to help regulate blood sugar levels. That said, combining these treatments can sometimes enhance blood sugar-lowering effects, which might raise the risk of hypoglycemia. To manage this, insulin doses are often adjusted, and regular blood sugar checks are strongly advised.
It’s important to talk to your healthcare provider before making any changes to your diabetes treatment plan. They can customize your medication approach to reduce risks and achieve the best possible outcomes.
What cardiovascular monitoring is recommended for patients using GLP-1 medications?
Patients taking GLP-1 receptor agonists should have regular cardiovascular check-ups to ensure their safety and achieve the best possible outcomes. Key areas to monitor include blood pressure, lipid profiles (LDL, HDL, and triglycerides), and body weight or BMI. These medications are known to help lower blood pressure, improve cholesterol levels, and support weight loss. Regular heart rate monitoring and, if necessary, an electrocardiogram (ECG) can help identify arrhythmias. Additionally, renal function tests (eGFR and serum creatinine) and HbA1c levels should be tracked to adjust dosing and monitor blood sugar levels effectively.
In some cases, clinicians may look for signs of heart failure by measuring natriuretic peptide levels or using echocardiography. This is particularly relevant since GLP-1 therapies have been shown to reduce hospitalizations related to heart failure. TrimRX incorporates these evidence-based monitoring practices into its personalized weight-loss programs. Their approach includes scheduled lab work, heart health evaluations, and ongoing clinical support for patients using medications such as semaglutide, tirzepatide, Mounjaro, Wegovy, and Ozempic.
Related Blog Posts

Transforming Lives, One Step at a Time
Keep reading
How to Adjust Weight Loss Goals on GLP-1 Medications
Adjust weight goals on GLP-1 meds by tracking body composition and labs, optimizing protein, activity, sleep, and working with your provider on dosing.
Falsified Mounjaro pens prompt urgent safety advisory
MHRA warns of counterfeit Mounjaro pens (batch D873576); stop use and check batch numbers for infection risk.
Novo Nordisk shares drop as Alzheimer’s hopes for weight-loss drug fade
Novo Nordisk’s semaglutide failed to slow Alzheimer’s in large trials, prompting shares to fall and expert reactions.



