GLP-1 vs. Other Medications: Interaction Risks

GLP-1 receptor agonists, like Semaglutide, Tirzepatide, and Liraglutide, are widely used for managing diabetes and weight loss. However, they can interact with other medications due to their effect on slowing digestion, which alters drug absorption. Key risks include:
- Hypoglycemia: Combining GLP-1 drugs with insulin or sulfonylureas can dangerously lower blood sugar.
- Oral Contraceptives: Tirzepatide can reduce their effectiveness by up to 55%, increasing pregnancy risks.
- Cardiovascular Drugs: Statins and warfarin are generally safe, but close monitoring is advised for drugs like digoxin.
- CNS/GI Medications: Opioids and anticholinergics can worsen GI side effects, while timing adjustments may be needed for some antidepressants or corticosteroids.
Key takeaway: Personalized treatment plans and regular monitoring are essential to safely combine GLP-1 therapies with other medications. Programs like TrimRX offer tailored support to minimize risks and optimize outcomes.
Ozempic Drug Interactions – What You NEED to Know Before Taking It! 💊

GLP-1 vs. Diabetes Medications: Interaction Risks
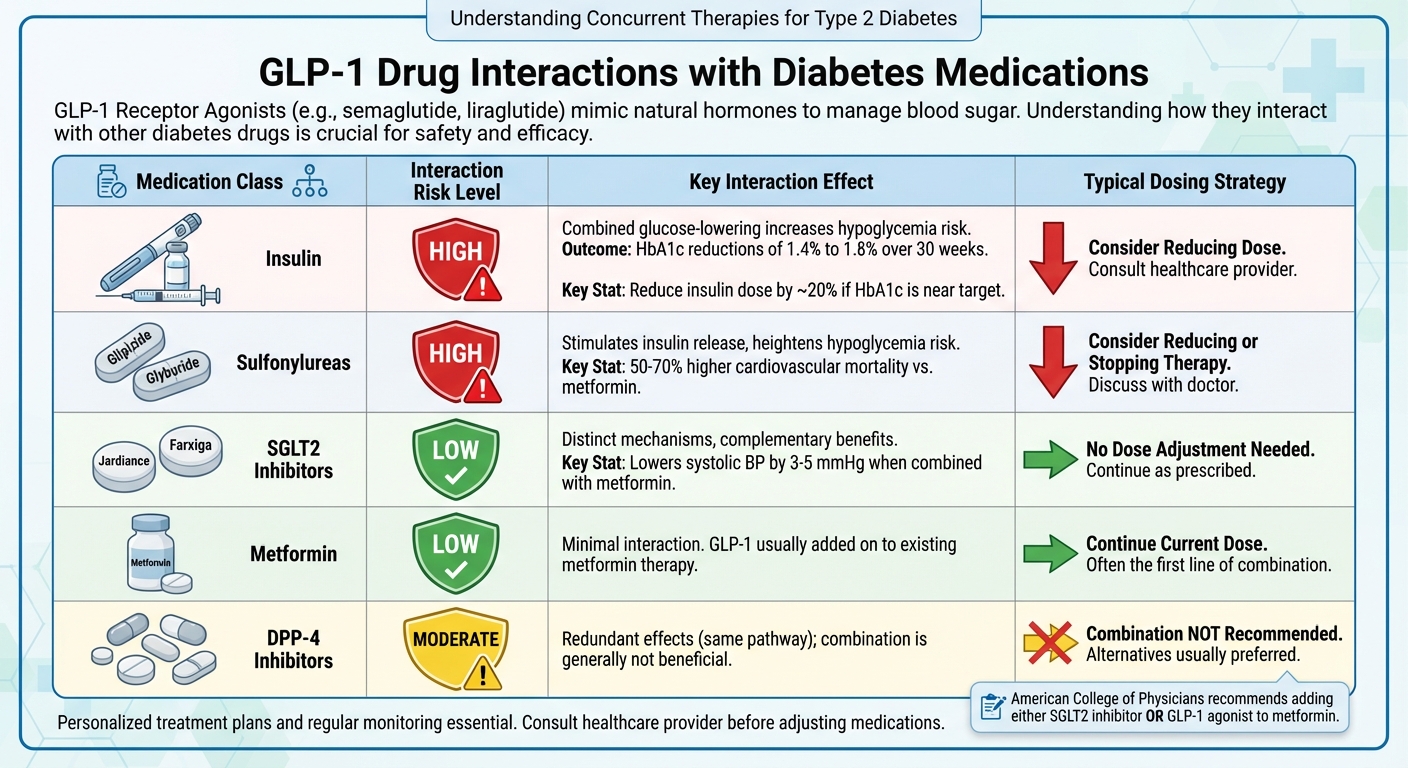
GLP-1 Drug Interactions with Diabetes Medications: Dosing Strategies and Risk Levels
Using GLP-1 receptor agonists alongside other diabetes medications requires careful attention to avoid complications like hypoglycemia. The primary concern is the combined glucose-lowering effects of these drugs. Below are some key interactions between GLP-1 medications and other diabetes treatments.
GLP-1 and Insulin
When GLP-1 medications are used with insulin, their combined glucose-lowering effects can significantly increase the risk of hypoglycemia. For example, in the SUSTAIN 5 clinical trial, patients with HbA1c levels of 8.0% or lower had their basal insulin doses reduced by 20% when starting semaglutide therapy to minimize the risk of low blood sugar. Even with these adjustments, semaglutide combined with basal insulin led to HbA1c reductions of 1.4% to 1.8% over 30 weeks. During the initial weeks of combined therapy, healthcare providers typically monitor blood sugar levels closely and adjust insulin doses as needed.
GLP-1 and Sulfonylureas
Sulfonylureas, like Glipizide and Glyburide, stimulate the pancreas to release more insulin, which can further lower blood sugar and heighten the risk of hypoglycemia when combined with GLP-1 drugs. Due to this risk, many healthcare providers reduce or even discontinue sulfonylurea therapy when starting GLP-1 treatment. It’s worth noting that cardiovascular mortality over two years was 50% to 70% higher in patients using sulfonylureas compared to those on metformin, according to research.
GLP-1 vs. SGLT2 Inhibitors and Other Non-Insulin Drugs
Medications like SGLT2 inhibitors (e.g., Jardiance, Farxiga), metformin, and DPP-4 inhibitors interact differently with GLP-1 drugs. SGLT2 inhibitors and metformin are often used alongside GLP-1 therapy because they work through distinct mechanisms, offering additional benefits like weight loss and improved cardiovascular health. For instance, combining SGLT2 inhibitors or GLP-1 agonists with metformin can lower systolic blood pressure by 3 to 5 mmHg. However, pairing GLP-1 drugs with DPP-4 inhibitors is generally avoided since both act on the same pathway, resulting in overlapping effects without meaningful added benefits. The American College of Physicians recommends adding either an SGLT2 inhibitor or a GLP-1 agonist to metformin when blood sugar control is insufficient, allowing for a more tailored treatment approach.
Here’s a quick summary of these interactions and recommended dosing strategies:
| Medication Class | Interaction with GLP-1 | Typical Dosing Strategy |
|---|---|---|
| Insulin | Higher risk of hypoglycemia | Reduce insulin dose by ~20% if HbA1c is near target |
| Sulfonylureas | Increased hypoglycemia risk | Consider reducing or stopping sulfonylurea therapy |
| SGLT2 Inhibitors | Low risk of hypoglycemia | No dose adjustment needed; provides additional benefits |
| Metformin | Minimal interaction | Continue current dose; GLP-1 is usually added on |
| DPP-4 Inhibitors | Redundant effects | Combination not recommended |
These insights highlight the importance of personalized treatment plans to balance efficacy and safety when combining GLP-1 drugs with other diabetes medications.
GLP-1 and Non-Diabetes Medications: Common Interactions
GLP-1 medications can influence how your body absorbs certain cardiovascular, hormonal, and CNS/GI drugs. Knowing these interactions is key to working with your healthcare provider to create a treatment plan that works for you. These effects differ depending on the drug type, making close collaboration with your doctor essential.
Cardiovascular Drugs
GLP-1 receptor agonists slow gastric emptying, which can delay the absorption of cardiovascular medications. For example, statins like atorvastatin and lovastatin may show delayed peak levels, but overall exposure remains unaffected. A study involving 966 patients on statins during exenatide trials found that lipid-lowering effects were comparable to those in the placebo group – 51% were on atorvastatin, and 31% on simvastatin.
Patients taking warfarin can usually continue their therapy without significant issues. Research shows that warfarin’s therapeutic range remains stable during GLP-1 treatment. While co-administration with lixisenatide or dulaglutide reduced warfarin’s peak concentration by 19% and 22% respectively, the International Normalized Ratio (INR) stayed consistent, and no bleeding events were reported.
For antihypertensive drugs like ACE inhibitors (lisinopril, ramipril), only minor changes in drug levels have been noted, which are generally not clinically significant. Routine blood pressure checks are usually enough. However, for medications with a narrow therapeutic index, such as digoxin, closer monitoring is necessary. Some GLP-1 drugs, particularly liraglutide, have been linked to reduced digoxin levels, so your doctor may monitor serum levels more closely, especially if you have kidney issues.
"Dose adjustments are probably not required for simultaneous use of GLP1RAs with oral medications. Still, results should be carefully generalized to cases of background kidney dysfunction or when using drugs with narrow therapeutic index." – Dr. Talia Diker Cohen, Rabin Medical Center
Interactions with hormonal medications also highlight the importance of tailored strategies.
Oral Contraceptives and Hormone Therapies
The gastric-emptying delay caused by GLP-1 medications can reduce the effectiveness of oral contraceptives, particularly with tirzepatide (Mounjaro/Zepbound). Tirzepatide decreases oral contraceptive exposure by about 20%, which increases the risk of pregnancy. This issue becomes even more critical since weight loss from GLP-1 therapy can naturally boost fertility, especially in women with conditions like PCOS.
"Tirzepatide is currently the only GLP-1 RA found to reduce the effects of oral contraceptives. Women of childbearing age using tirzepatide should be advised to switch to a non-oral contraceptive method or add a barrier method." – Specialist Pharmacy Service (SPS)
For patients on tirzepatide, healthcare providers recommend switching to non-oral contraceptives or adding a barrier method (like condoms) for four weeks after starting the drug and four weeks after each dose increase. Other GLP-1 drugs also affect oral contraceptives to varying degrees. For example, exenatide reduces the peak concentration of ethinyl estradiol by 15% to 45%, depending on timing, while liraglutide decreases it by 12%.
Timing strategies can help manage these interactions. For exenatide, take oral contraceptives at least one hour before your GLP-1 injection. With lixisenatide, take them either one hour before or 11 hours after your GLP-1 dose. Non-oral options like IUDs, implants, patches, vaginal rings, and injections bypass the digestive system entirely and are unaffected by GLP-1 medications.
CNS and GI Motility Medications
GLP-1 interactions with CNS and GI medications often require a personalized approach. Prokinetic agents like erythromycin can counteract the gastric-slowing effects of GLP-1 drugs, impacting both gastric emptying and glycemic control. If you need long-term prokinetic therapy, GLP-1 medications might not be the best fit.
Opioids and anticholinergics can further slow GI motility, potentially leading to severe constipation or symptoms of gastroparesis. For antidepressants like SSRIs, absorption may be delayed, but dose adjustments are rarely needed. However, it’s a good idea to watch for nausea or other GI side effects.
Oral corticosteroids can also pose challenges. Delayed absorption could interfere with diagnostic tests like the dexamethasone suppression test. Some case reports suggest that patients on chronic hydrocortisone therapy may experience adrenal insufficiency symptoms when starting GLP-1 drugs. Adjusting the timing of your steroid dose – taking it before meals and your GLP-1 dose after meals – could help address this.
| CNS/GI Drug Class | Potential Interaction with GLP-1 | Clinical Recommendation |
|---|---|---|
| Prokinetics | Counteracts GLP-1’s gastric-slowing effects | Avoid combining if GLP-1 efficacy is a priority |
| Opioids/Anticholinergics | May worsen slowed GI motility and constipation | Monitor for severe GI side effects |
| SSRIs/Antidepressants | Delayed absorption; possible GI side effects | Monitor mood and GI tolerance; no routine dose adjustment |
| Oral Corticosteroids | Delayed absorption; test inaccuracies | Adjust timing; repeat tests if results are unclear |
These interactions highlight the need for customized approaches when starting GLP-1 therapy, ensuring that your treatment plan aligns with your specific health needs.
sbb-itb-e2779c3
When Dose Adjustments Are Not Required
GLP-1 medications slow down how quickly the stomach empties, which delays the time it takes for a drug to reach peak concentration. However, the total drug exposure (measured as AUC) remains the same. This consistency means that routine dose adjustments are generally unnecessary. Clinical studies back this up, showing steady pharmacokinetic profiles with GLP-1 therapies.
General Findings from Studies
In one clinical study involving 31 participants, researchers found that the AUC ratios for common medications like metformin, warfarin, atorvastatin, and digoxin stayed within the bioequivalence range of 0.80–1.25 when taken alongside semaglutide. This indicates that dose adjustments for these drugs are not typically needed. As noted by Hausner’s team:
"No clinically significant pharmacokinetic or pharmacodynamic interactions were identified… This suggests that no dose adjustments should be required when semaglutide is administered concomitantly with these medications."
Other findings support this consistency. For example, while acetaminophen shows a delay in reaching peak concentration, its overall bioavailability remains unchanged. Similarly, a 2009 study on ACE inhibitors like lisinopril and ramipril, conducted with 22 patients who had mild-to-moderate hypertension, revealed that exenatide did not impact the steady-state pharmacokinetics of lisinopril. The AUC ratio was 0.97 (90% CI: 0.90–1.04). Although it’s a good idea to monitor blood pressure when starting GLP-1 therapy, adjusting doses of these medications is rarely necessary.
Over-the-Counter Medications and Supplements
The same principles apply to over-the-counter medications. Most, including acetaminophen and dietary supplements, do not require dose adjustments when taken with GLP-1 therapies. However, medications that rely on a rapid onset, like fast-acting pain relievers, might take longer to work because of the delayed gastric emptying. If this delay affects immediate relief, it’s wise to consult your doctor for guidance.
Personalized Solutions for Managing Interaction Risks
When it comes to managing GLP-1 therapy alongside other medications, there’s no universal formula. Every individual’s medical history, organ function, and medication regimen must be carefully evaluated to reduce interaction risks while ensuring the treatment remains effective.
Although many medications don’t require dose adjustments with GLP-1 therapy, individual circumstances often call for tailored approaches to address specific risks.
Customizing GLP-1 Doses for Safety and Effectiveness
While most medications retain stable exposure levels during GLP-1 therapy, unique clinical factors may require adjustments in dosage or timing.
Dose titration is essential for avoiding adverse interactions. For instance, when initiating GLP-1 therapy, a gradual reduction in insulin doses can help prevent diabetic ketoacidosis. Extra caution is necessary for patients on medications with narrow therapeutic windows, such as tacrolimus. Notably, around 30% of solid organ transplant recipients experience post-transplant diabetes[1].
Timing adjustments can also play a critical role. For example, women taking oral contraceptives should take them at least one hour before an exenatide injection to maintain their effectiveness. Switching to transdermal estrogen may be a better option for those on oral hormone replacement therapy to avoid absorption issues. Additionally, people on time-sensitive medications like levodopa should work closely with their healthcare providers to monitor their response and adjust timing if needed.
Patients with impaired liver or kidney function need extra care, especially when using tirzepatide, which contains benzyl alcohol and may increase the risk of metabolic acidosis. It’s also crucial to inform your healthcare team about GLP-1 therapy before undergoing surgery to manage aspiration risks effectively.
How TrimRX Supports Individualized Care
TrimRX offers personalized weight loss programs that take into account each patient’s unique medication needs. Through customized consultations, medical professionals thoroughly review your medication list, organ function, and health background before prescribing GLP-1 medications like Semaglutide or Tirzepatide. This proactive assessment helps identify potential risks early.
The platform provides unlimited check-ins, giving you continuous support as your GLP-1 dosage changes or your medication regimen evolves. From guidance on timing strategies to monitoring recommendations and advice on when to involve your primary care physician, TrimRX ensures your treatment plan adjusts to your body’s needs. This personalized approach highlights the importance of managing GLP-1 interactions effectively.
Final Thoughts on GLP-1 and Medication Interactions
Pharmacokinetic studies indicate that about 73% of studied interactions remain within safe limits[1], though some cases require careful monitoring by healthcare professionals. Regular blood glucose checks become especially important when modifying GLP-1 or insulin doses.
The cornerstone of safe GLP-1 therapy is open communication with your healthcare team. Share details about all the medications you take, including over-the-counter products and supplements. With proper monitoring and personalized adjustments, most interaction risks can be managed without compromising your weight loss journey.
FAQs
Do GLP-1 medications interact with other drugs?
GLP-1 receptor agonists, like semaglutide and tirzepatide, can slow down how quickly your stomach empties. This is part of their glucose-lowering effects. While this delay doesn’t usually change the total amount of a medication absorbed, it can impact the timing of absorption for certain drugs. Medications with a narrow therapeutic window or those that need to act quickly – like warfarin, oral contraceptives, or acetaminophen – might require closer attention.
For most medications, dose adjustments aren’t necessary. However, it’s a good idea to monitor how your body reacts, especially if you’re taking anticoagulants, antiepileptics, or hormone-based treatments. TrimRX’s personalized weight-loss programs include consultations to review your current medications and address possible interactions, helping ensure your treatment plan stays safe and effective.
What should I know about using GLP-1 medications with oral contraceptives?
If you’re using GLP-1 receptor agonists like tirzepatide, keep in mind that these medications can slow down how quickly your stomach empties. This can potentially make oral contraceptives less effective. To ensure you’re fully protected, you might want to use a barrier method or switch to a non-oral contraceptive for about four weeks after starting or changing your dose of GLP-1 medication. Be sure to talk to your healthcare provider to figure out the best approach for your needs.
What should I know about combining GLP-1 medications with insulin or sulfonylureas?
When combining GLP-1 receptor agonists with insulin or sulfonylureas, the chance of experiencing hypoglycemia (low blood sugar) goes up. To address this, regular monitoring of your blood sugar levels is essential. Your healthcare provider may need to adjust the doses of insulin or sulfonylureas to keep your treatment safe and effective.
It’s crucial to talk to your doctor before making any changes to your medication. They can offer tailored advice to help manage your condition while minimizing risks.
Related Blog Posts

Transforming Lives, One Step at a Time
Keep reading
How to Adjust Weight Loss Goals on GLP-1 Medications
Adjust weight goals on GLP-1 meds by tracking body composition and labs, optimizing protein, activity, sleep, and working with your provider on dosing.
Falsified Mounjaro pens prompt urgent safety advisory
MHRA warns of counterfeit Mounjaro pens (batch D873576); stop use and check batch numbers for infection risk.
Novo Nordisk shares drop as Alzheimer’s hopes for weight-loss drug fade
Novo Nordisk’s semaglutide failed to slow Alzheimer’s in large trials, prompting shares to fall and expert reactions.



