Common Misconceptions About GLP-1 Weight Loss

GLP-1 medications, such as Wegovy and Zepbound, are gaining attention for weight loss, but they’re often misunderstood. These medications help regulate hunger and improve insulin function, but they’re not a quick fix. Success requires combining them with healthy eating, exercise, and long-term commitment. Key points to know:
- Not effortless: Lifestyle changes are essential for meaningful results.
- Not instant or permanent: Weight loss is gradual, and stopping the medication often leads to weight regain.
- Side effects are temporary: Digestive symptoms like nausea usually subside over time.
- Not for everyone: Certain health conditions or life stages may make these drugs unsuitable.
- Different options: Medications vary in dosing, formulation, and effectiveness.
GLP-1s are tools, not solutions. They work best with medical guidance and consistent effort.
GLP-1s Explained: Science, Myths & The Truth About Weight Loss Injections
Myth 1: GLP-1 Medications Make Weight Loss Effortless
A common misunderstanding about GLP-1 medications is that they magically make weight loss effortless. In reality, these medications are just tools – they support your journey but don’t replace the need for healthy eating and exercise. Clinical trials proving their effectiveness also included education on nutrition and physical activity, which are essential for achieving meaningful results.
"All the clinical trials that showed these medications working also included education on eating and exercise. We see much greater success when lifestyle changes are part of the plan." – Patrick Welch, PharmD, BCACP, Intermountain Health
This highlights the importance of staying actively involved in your weight loss efforts.
The FDA-approved guidelines for GLP-1 medications specifically recommend combining them with a reduced-calorie diet and increased physical activity. For example, patients taking Wegovy (semaglutide 2.4 mg) achieved an average weight loss of 14.9% after 68 weeks when paired with lifestyle changes. Similarly, tirzepatide (Zepbound) demonstrated up to 22.5% weight loss in a 72-week trial with the same approach.
Why Lifestyle Changes Are Key
GLP-1 medications help by curbing hunger and enhancing feelings of fullness, but they don’t determine your food choices or activity levels. Making lifestyle adjustments is essential to reinforce the medication’s effects and address the behavioral aspects of weight management. Without these changes, the results are often short-lived.
Physical activity plays a critical role, especially in preserving muscle mass. Rapid weight loss can result in losing 15–25% of lean muscle if resistance training and adequate protein intake aren’t part of the plan. Strength training just a few times a week can help maintain muscle, bone density, and metabolism while the medication works on appetite regulation.
"The amount of diet and exercise will vary among users, leading to various degrees of weight loss. However, consistent physical activity is vital to achieve and maintain the desired weight loss." – HaVy Ngo-Hamilton, PharmD, BuzzRx
Eating habits are equally important. Focusing on lean proteins, fiber-rich vegetables, and healthy fats can support your metabolism while also managing common side effects like nausea or constipation. Staying hydrated and steering clear of ultra-processed foods, such as sugary snacks and fried items, can make a world of difference in how you feel while on the medication.
These lifestyle changes are essential because managing obesity requires a long-term commitment.
Understanding Obesity as a Chronic Condition
It’s crucial to recognize that obesity is a chronic medical condition, not a temporary issue that can be solved with a quick fix. Just like managing high blood pressure or diabetes, treating obesity requires ongoing effort and support. GLP-1 medications address biological factors like hunger cues and insulin function, but they don’t eliminate the need for sustainable healthy habits.
"By enhancing the effects of GLP-1, these medications help to reduce hunger and increase feelings of fullness, leading to reduced caloric intake without the need for extreme dieting or willpower." – Laura Buford, MD
Without building solid habits, weight often returns once the medication is stopped. Hunger cues typically come back quickly, which is why establishing a foundation of healthy eating and regular exercise during treatment is vital for maintaining long-term results.
Myth 2: GLP-1 Medications Deliver Instant, Permanent Results
GLP-1 medications don’t promise instant or permanent weight loss. Instead, they require patience and a long-term approach to achieve meaningful results.
Weight loss with these medications happens gradually. Patients typically begin with a low dose – usually 0.25 mg of semaglutide – and increase the dosage every four weeks. This slow progression helps minimize gastrointestinal side effects. Reaching the full maintenance dose often takes 16 to 20 weeks. It’s important to understand that these medications manage a chronic condition, not provide a quick fix. Once the treatment is stopped, the effects are reversed fairly quickly.
What Happens When Medication Stops
When GLP-1 medications are discontinued, weight regain is a common outcome. These drugs are effective only while active in your system, and stopping treatment allows hunger and fullness signals to revert to their pre-treatment state. Many patients report experiencing a rapid return of hunger within days of their last dose.
"Stopping weight loss drugs can feel like ‘jumping off a cliff’… The food noise comes back as quickly as the next day." – Dr. Hussain Al-Zubaidi, Lifestyle GP
Clinical studies back this up. On average, patients regain about 60% of the weight they lost within a few months to a year after stopping the medication, even when maintaining healthy habits like proper nutrition and exercise. For example, in the STEP 4 trial, participants who stayed on semaglutide for 68 weeks lost an additional 7.9% of their body weight. In contrast, those switched to a placebo regained 6.9%. Another study found that participants regained an average of 11.6% of their body weight within a year after stopping treatment.
This weight regain is partly due to metabolic changes that slow down your metabolism during weight loss, making it harder to maintain progress. Additionally, withdrawal symptoms like increased appetite, binge eating, and blood sugar spikes in diabetic patients can make the transition even more challenging. All of this highlights the importance of a long-term treatment plan.
The Importance of Long-Term Treatment
Sustaining weight loss typically requires continued use of GLP-1 medications, combined with long-term lifestyle changes. Think of it as similar to managing other chronic conditions, where daily medication is often necessary.
"Obesity is a chronic disease so we should treat it the same way as, say, high blood pressure, where you just take those drugs every single day for the rest of your life." – Suzanne Rose, PhD, Executive Director of Research, Stamford Health
If you’re considering stopping the medication, it’s essential to work with your healthcare provider on a structured plan. Gradually tapering the dose can help your body adjust and may reduce the risk of rapid weight regain. Regular check-ins with your provider can also help maintain cardiometabolic benefits.
However, the cost of treatment can be a significant hurdle. Without insurance, monthly expenses for brand-name GLP-1 medications can exceed $1,300, and many insurers don’t cover these drugs specifically for weight loss. This financial reality makes it important to plan carefully for the long-term commitment these medications require.
Myth 3: GLP-1 Medications Cause Permanent Stomach Damage
A common worry about GLP-1 medications is that they might cause lasting harm to your digestive system. This concern likely stems from how frequently gastrointestinal side effects occur. However, this fear is based on a misunderstanding of how these medications function. While they can cause temporary digestive symptoms, these effects are not signs of permanent damage.
GLP-1 medications work by slowing gastric emptying, meaning they reduce the speed at which food moves from your stomach to your small intestine. This mechanism helps you feel full for longer periods. The nausea, bloating, or other digestive symptoms some people experience are temporary reactions to this slowed digestion – not evidence of lasting harm.
Common Side Effects and Their Causes
The temporary slowing of gastric emptying explains many of the common side effects of GLP-1 medications. Gastrointestinal symptoms are the most frequently reported issues, with nausea being the most common. For example, clinical trials for semaglutide at a 2.4 mg dose showed that 44.2% of participants experienced nausea, compared to 17.4% in the placebo group. Other side effects, such as diarrhea, vomiting, and constipation, are also relatively common.
Fortunately, these symptoms are usually mild or moderate and tend to decrease over time as your body adjusts. In a clinical trial studying liraglutide, nausea affected 24.7% of participants at week 4, but this number dropped to just 5.5% by week 56.
"GI AEs typically occur during initiation and uptitration, appearing as transient, mild-to-moderate symptoms." – Laura Schalliol, PharmD, BCACP, BCGP, Professor of Pharmacy Practice
In fact, 94% of adverse events reported in major clinical trials were mild or moderate in severity. Only 5% to 10% of patients discontinue treatment due to side effects. While rare complications like gastroparesis (stomach paralysis) or pancreatitis can occur, they are uncommon.
To reduce digestive discomfort, try eating smaller, more frequent meals and avoid greasy, high-fat, or heavily processed foods – especially on the days you take your injection. Staying well-hydrated and practicing mindful eating (stopping when you feel full) can also help manage these temporary symptoms.
Safety Backed by Research
The safety of GLP-1 medications is well-supported by extensive research. These drugs have been used to treat type 2 diabetes for nearly two decades, with the first GLP-1 medication, exenatide, gaining FDA approval in 2005. This long history of use provides strong evidence of their safety when prescribed and monitored by healthcare professionals.
"GLP-1 agonists have a favorable safety profile, with most side effects being mild and temporary. Common side effects include nausea, diarrhea and constipation, which typically subside as the body adjusts to the medication." – Laura Buford, MD
Importantly, GLP-1 medications only temporarily affect gastric emptying while you are actively taking them. They do not harm tissue or permanently alter the structure or function of your digestive system. Once you stop the medication, your gastric emptying rate returns to normal.
Always use GLP-1 medications under the guidance of a healthcare provider. If you’re concerned about digestive side effects or have a history of gastrointestinal issues, discuss these with your doctor before starting treatment. For additional support, TrimRX offers personalized assistance to help you manage your therapy safely and effectively.
Myth 4: GLP-1 Medications Work Like Bariatric Surgery
GLP-1 medications and bariatric surgery operate in entirely different ways. Bariatric surgery physically changes your digestive system, while GLP-1 medications rely on hormonal signaling to achieve their effects.
Bariatric procedures like gastric bypass or sleeve gastrectomy involve permanent structural changes. For instance, these surgeries either create a small stomach pouch (~30 mL) or remove up to 70% of the stomach. This reduction in stomach size limits how much food you can eat. On the other hand, GLP-1 medications don’t alter the stomach’s structure at all. This distinction is key when comparing their mechanisms and long-term impacts.
The outcomes also vary. Bariatric surgery often leads to a 60% to 70% reduction in excess body weight, while GLP-1 medications like semaglutide typically result in a 15-20% total body weight loss. For example, in a 68-week clinical trial, semaglutide users experienced an average weight loss of 15.8%, with 86% of participants achieving clinically meaningful results.
How GLP-1s Affect Hunger and Satiety
GLP-1 medications help regulate appetite by mimicking a hormone your body naturally produces. These medications target receptors in the brain – specifically in the hypothalamus and hindbrain – to curb appetite and reduce constant thoughts about food, often referred to as "food noise."
"Lots of people describe it as decreasing ‘food noise,’ which means how much you think about food and how much you crave different foods." – Evan Nadler, MD, MBA, Adjunct Associate Professor, George Washington University
sbb-itb-e2779c3
Myth 5: GLP-1 Medications Are Only for Type 2 Diabetes
Although GLP-1 medications were initially created to manage diabetes, they now have FDA approval for chronic weight management in people without diabetes.
Formulations such as Wegovy (semaglutide), Zepbound (tirzepatide), and Saxenda (liraglutide) are approved for adults with a BMI of 30 or higher, or 27 and above if accompanied by conditions like high blood pressure or cholesterol. These medications are also approved for pediatric patients aged 12 and older who have obesity. Beyond helping with weight loss, these drugs offer additional health benefits, broadening their role in medical care.
Broader Applications of GLP-1 Medications
GLP-1 medications aren’t just about weight management – they also contribute to better cardiovascular health. Certain formulations are FDA-approved to lower the risk of serious cardiovascular events, such as heart attacks and strokes, in adults with heart disease who are overweight or obese. This dual benefit makes them an important option for tackling multiple health issues.
For example, Ozempic and Mounjaro are approved for managing Type 2 diabetes, while Wegovy and Zepbound are specifically approved for weight loss. Although these medications share active ingredients, their dosages and FDA-approved uses differ. In a major step forward, the FDA approved the first generic liraglutide for weight loss in August 2025, making these treatments more affordable.
"With this approval, and by launching a generic for Saxenda, we will provide patients in the U.S. the first ever generic GLP-1 product specifically indicated for weight loss." – Ernie Richardsen, Senior Vice President, Teva Pharmaceuticals
Despite their potential, only about 4% of eligible individuals currently receive these prescriptions. High costs, stigma, and limited provider familiarity often stand in the way. Expanding awareness of their benefits could help more people access these treatments.
Myth 6: All GLP-1 Medications Are the Same
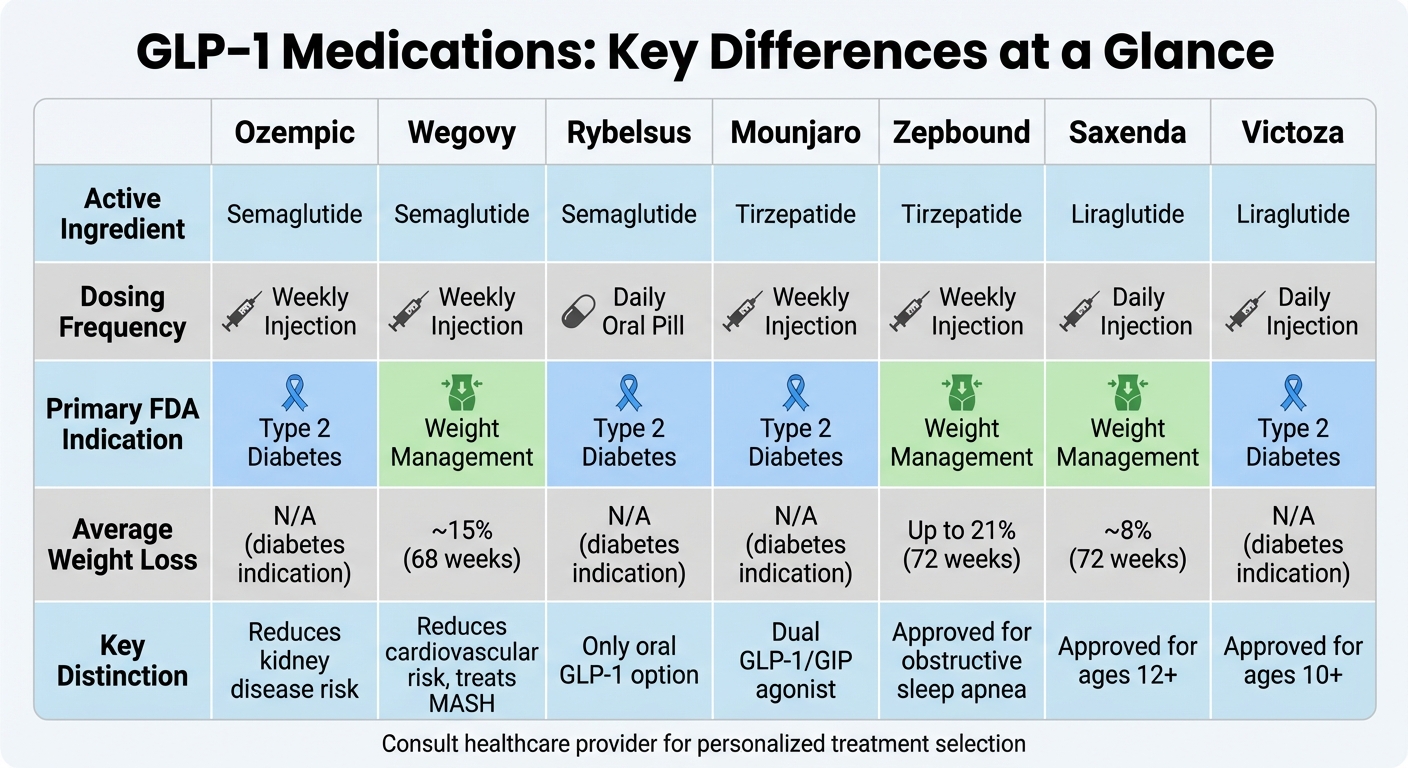
GLP-1 Medications Comparison Chart: Dosing, Uses, and Key Differences
It’s easy to assume that all GLP-1 medications work the same way, but there are important differences that set them apart. These medications, which mimic hormones that regulate appetite, vary in their formulation, dosing schedules, and approved uses. In short, they’re not interchangeable.
Take semaglutide, for example. It’s sold under the names Ozempic and Wegovy, but these aren’t identical products. Ozempic is designed for managing type 2 diabetes, while Wegovy is specifically approved for weight loss. Each comes with its own dosing and indications.
Comparing Popular GLP-1 Medications
How these medications are delivered also differs. Most require weekly injections, but some, like Saxenda and Victoza, need daily injections. If injections aren’t your thing, Rybelsus offers an alternative as the only oral tablet in the GLP-1 category.
There are also differences in how these medications work and their effectiveness. Tirzepatide, sold as Mounjaro for diabetes and Zepbound for weight management, is a dual GLP-1/GIP receptor agonist. Research suggests it might be more effective than medications that target only GLP-1. For example, clinical trials show the following average weight loss results over 72 weeks:
- Saxenda: Around 8% of body weight
- Wegovy: Nearly 15%
- Zepbound: Up to 21%
But it’s not just about weight loss. Some GLP-1 medications come with additional FDA-approved benefits. For instance:
- Wegovy reduces the risk of major cardiovascular events by 20% and is approved for treating metabolic dysfunction-associated steatohepatitis (MASH) with liver scarring.
- Ozempic can lower the risk of worsening kidney disease in adults with type 2 diabetes and chronic kidney disease.
- Zepbound is approved for managing obstructive sleep apnea in adults with obesity.
Here’s a quick breakdown of common GLP-1 medications:
| Medication | Active Ingredient | Dosing Frequency | Primary FDA Indication | Key Distinction |
|---|---|---|---|---|
| Ozempic | Semaglutide | Weekly Injection | Type 2 Diabetes | Reduces kidney disease risk |
| Wegovy | Semaglutide | Weekly Injection | Weight Management | Reduces cardiovascular risk, treats MASH |
| Rybelsus | Semaglutide | Daily Oral Pill | Type 2 Diabetes | Only oral GLP-1 option |
| Mounjaro | Tirzepatide | Weekly Injection | Type 2 Diabetes | Dual GLP-1/GIP agonist |
| Zepbound | Tirzepatide | Weekly Injection | Weight Management | Approved for obstructive sleep apnea |
| Saxenda | Liraglutide | Daily Injection | Weight Management | Approved for ages 12 and up |
| Victoza | Liraglutide | Daily Injection | Type 2 Diabetes | Approved for ages 10 and up |
These distinctions highlight the importance of a personalized approach to treatment. Choosing the right medication depends on your specific health needs and goals. If you’re looking for expert guidance, programs like TrimRX can help tailor a weight loss plan that works for you.
Myth 7: GLP-1 Medications Are Safe for Everyone
GLP-1 medications can help with weight loss, but they aren’t a one-size-fits-all solution. Certain health conditions and life circumstances can make these drugs unsuitable or even dangerous. Knowing who should avoid them is critical for safe and effective treatment.
Who Should Avoid GLP-1 Medications
Genetic and Cancer Concerns
If you or your family has a history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia type 2 (MEN 2), GLP-1 medications come with an increased risk of thyroid C-cell tumors and should be avoided.
Pregnancy and Breastfeeding
Women planning to conceive should stop taking semaglutide at least two months before trying to get pregnant to minimize potential risks to the fetus. These medications are also not recommended during breastfeeding.
Pancreatic and Gallbladder Conditions
People with a history of acute pancreatitis or gallbladder disease may face heightened risks when using GLP-1 medications. For instance, clinical trials revealed that 1.6% of patients on semaglutide developed gallstones, compared to 0.7% of those on a placebo. Additionally, about 6.8% of patients discontinue GLP-1 treatment due to side effects, primarily gastrointestinal issues.
Pre-Surgery Precautions
Because GLP-1 medications slow down gastric emptying, they can increase the risk of aspiration during general anesthesia. Doctors typically recommend stopping these medications several days before surgery.
Other At-Risk Groups
GLP-1 medications are generally not suitable for individuals with severe gastrointestinal disorders like gastroparesis, those with type 1 diabetes (as these drugs are approved only for type 2 diabetes and obesity), and people with a history of suicidal thoughts, active eating disorders, or heavy alcohol use. These risks highlight the importance of professional guidance.
The Importance of Medical Supervision
Taking GLP-1 medications without proper medical oversight can lead to serious complications. By July 31, 2025, the FDA had received 605 reports of adverse events tied to compounded semaglutide and 545 reports related to compounded tirzepatide. Many of these incidents involved dosing errors that resulted in hospital visits.
"Many direct-to-consumer brands don’t have full access to a patient’s medical history. That can lead to gaps in treatment, making the medication less effective or even unsafe." – Patrick Welch, PharmD, BCACP, Intermountain Health
A licensed healthcare provider plays a vital role in reviewing your medical history, assessing risk factors, and monitoring your treatment. If you experience severe abdominal pain, jaundice, or difficulty passing gas while on these medications, seek immediate medical attention, as these symptoms could indicate serious issues like pancreatitis or gallbladder complications.
Personalized programs like TrimRX offer the medical oversight needed to safely use GLP-1 medications, ensuring you stay on track and address any concerns that may arise.
Conclusion
GLP-1 medications have emerged as a promising tool for addressing obesity as a chronic condition, but they’re far from the quick fix often portrayed on social media. These medications deliver the best results when combined with balanced nutrition, consistent strength training, and regular medical oversight – not as a standalone approach.
Dispelling common myths about these treatments can help set more realistic expectations. Weight loss tends to be steady, around 1–2 pounds per week, requiring patience and long-term dedication. Temporary side effects like nausea are generally manageable and don’t signal permanent harm.
"Weight loss [on these medications] is not just about eating less. It is about supporting hormonal and metabolic changes." – Jamie Mills, RDN
Professional guidance plays a key role in safe and effective use. Healthcare providers are essential for determining the right dosage, tracking progress, and addressing any concerns along the way. Tailored programs, such as those offered by TrimRX, highlight the importance of personalized care for achieving sustainable results.
Successfully managing obesity involves more than just medication – it requires the right tools, expert support, and a commitment to long-term goals.
FAQs
Can GLP-1 medications alone help me maintain long-term weight loss?
GLP-1 medications, like Semaglutide and Tirzepatide, have shown the potential to help people lose between 5% and 15% of their body weight. Even better, these results can often be maintained for at least a year. But here’s the catch: studies suggest that without pairing these medications with healthy lifestyle habits – like eating a balanced diet, staying active, and making behavioral changes – weight regain is a common outcome.
To make the results stick, it’s crucial to think of GLP-1 medications as just one piece of a larger weight loss strategy. Programs like TrimRX can create personalized plans that combine medication with the tools and guidance you need to build lasting, healthy habits.
What happens if you stop taking GLP-1 medications suddenly?
When you stop taking GLP-1 medications suddenly, it can result in rapid weight regain. Research indicates that as much as 60–70% of the weight lost may come back within just a few months. This happens largely because appetite returns to previous levels, and the metabolic improvements gained during treatment are no longer present.
To maintain your progress and avoid setbacks, it’s crucial to collaborate with your healthcare provider. Together, you can develop a plan for transitioning off the medication gradually. Pairing this with ongoing lifestyle changes can help support lasting results.
Are GLP-1 medications right for everyone trying to lose weight?
GLP-1 medications have shown strong potential for aiding weight loss, but they aren’t the right choice for everyone. Initially developed to manage type 2 diabetes, these medications help by curbing appetite, slowing digestion, and keeping blood sugar levels in check. While such effects can lead to noticeable weight loss, they are only prescribed for individuals who meet specific medical requirements.
Before starting GLP-1 therapy, a healthcare provider will carefully review your medical history to ensure it’s a safe option for you. Certain conditions, like a personal or family history of medullary thyroid cancer or multiple endocrine neoplasia type 2, can make these medications unsuitable. Additionally, some individuals may experience side effects, such as nausea or digestive issues, which often require adjusting the dosage under medical supervision.
For those who qualify, TrimRX provides customized weight loss plans that incorporate GLP-1 medications such as semaglutide or tirzepatide. These plans also include personalized consultations, free medication delivery, and ongoing support to help you succeed. Talk to a qualified provider to find out if GLP-1 therapy aligns with your weight loss goals.
Related Blog Posts

Transforming Lives, One Step at a Time
Keep reading
How to Adjust Weight Loss Goals on GLP-1 Medications
Adjust weight goals on GLP-1 meds by tracking body composition and labs, optimizing protein, activity, sleep, and working with your provider on dosing.
Falsified Mounjaro pens prompt urgent safety advisory
MHRA warns of counterfeit Mounjaro pens (batch D873576); stop use and check batch numbers for infection risk.
Novo Nordisk shares drop as Alzheimer’s hopes for weight-loss drug fade
Novo Nordisk’s semaglutide failed to slow Alzheimer’s in large trials, prompting shares to fall and expert reactions.



