Why GLP-1 Medications Cause GI Issues

GLP-1 medications like semaglutide (Ozempic, Wegovy), liraglutide (Saxenda, Victoza), and tirzepatide (Mounjaro, Zepbound) are effective for managing type 2 diabetes and aiding weight loss, but up to 40% of patients experience gastrointestinal (GI) side effects. These include nausea, vomiting, bloating, diarrhea, and constipation, often linked to how these drugs slow digestion and alter intestinal movement. Symptoms are most common during the first few weeks or after dose increases and tend to improve over time.
Key Points:
- GI symptoms arise from delayed stomach emptying and changes in intestinal activity.
- Higher doses and rapid dose escalation increase the likelihood of side effects.
- Nausea and vomiting are the most reported, with rates peaking early in treatment.
- Diarrhea and constipation occur due to slowed intestinal transit and reduced enzyme secretion.
- Gallbladder issues, including gallstones, may occur, especially during rapid weight loss.
Managing Side Effects:
- Start with low doses and increase gradually.
- Eat small, low-fat meals and stay hydrated.
- Avoid lying down after meals and consider light activity.
- Seek medical help for severe or persistent symptoms, like abdominal pain or dehydration.
While these side effects can be uncomfortable, they often improve with time and proper dose adjustments. Working closely with a healthcare provider helps balance treatment benefits with tolerable side effects.
GLP1 and GIP Receptor Agonists Effect on the GI Tract
GLP-1 Medications and Their GI Side Effects
GLP-1 Medication Side Effects: Prevalence and Risk Comparison
What Are GLP-1 Receptor Agonists?
GLP-1 receptor agonists are medications that imitate the effects of glucagon-like peptide-1, a hormone released after eating. These drugs help regulate blood sugar by triggering insulin release and suppressing glucagon. They also slow down how quickly food moves through the stomach and signal the brain to reduce hunger and increase feelings of fullness.
The FDA has approved these medications for two primary uses: managing type 2 diabetes and aiding in chronic weight management for individuals with obesity or those who are overweight and have related health conditions. Common examples include semaglutide (Ozempic, Wegovy), tirzepatide (Mounjaro, Zepbound), liraglutide (Saxenda, Victoza), and dulaglutide (Trulicity). Tirzepatide is unique because it targets both GLP-1 and glucose-dependent insulinotropic polypeptide (GIP) receptors, making it a dual agonist.
This mechanism of action explains why these medications often affect digestion as well.
Common GI Side Effects
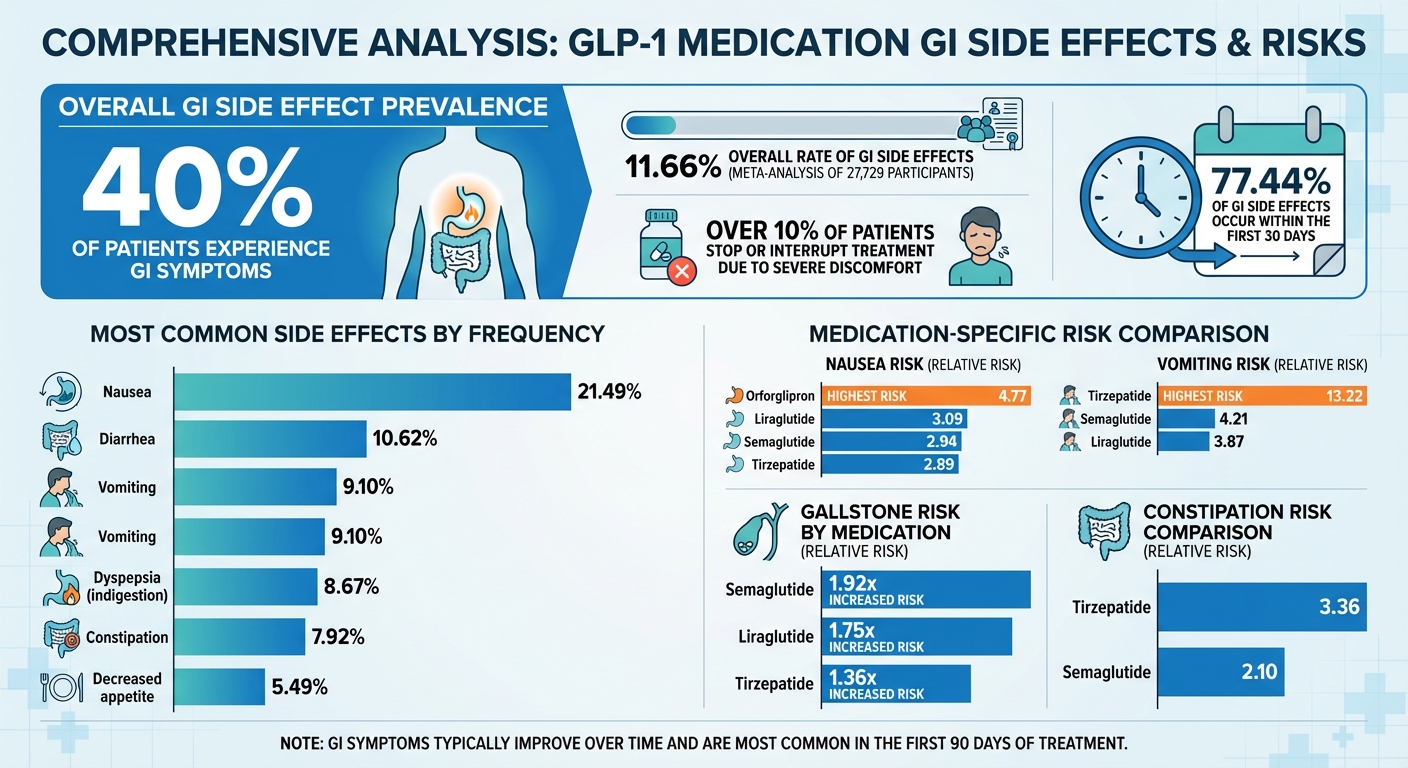
About 40% of patients experience gastrointestinal (GI) symptoms while using GLP-1 receptor agonists. These side effects are typically mild to moderate and are most common during the first few weeks of treatment or after a dose increase. The most frequently reported issues include:
- Nausea: 21.49% of patients
- Diarrhea: 10.62%
- Vomiting: 9.10%
- Dyspepsia (indigestion): 8.67%
- Constipation: 7.92%
- Decreased appetite: 5.49%
While many tolerate these medications well, over 10% of patients stop or interrupt treatment due to severe discomfort. A meta-analysis of 27,729 participants found the overall rate of GI side effects to be 11.66%. Additionally, the FDA has issued warnings about ileus (bowel obstruction) after receiving 90 postmarketing reports.
These statistics highlight why GI issues often become more pronounced with higher doses.
Why Higher Doses Cause More GI Problems
GI side effects tend to worsen at higher doses because of increased receptor stimulation. Higher doses amplify GLP-1 receptor activity in areas of the brain, like the Area Postrema, which is responsible for triggering nausea. Studies show a direct link between the concentration of the drug in the bloodstream and the frequency of nausea. For instance, in the STEP 2 trial, nausea rates rose from 5% at the initial 0.25 mg dose to 15% when patients reached the 2.4 mg dose of semaglutide.
"The GLP-1R monoagonists displayed a significant positive correlation between Css [circulating concentration] and nausea, which is not observed for the GIPR/GLP-1R dual-agonist." – Jonathan D. Douros, PhD, Indiana Biosciences Research Institute
Another contributing factor is how quickly doses are increased. Rapid dose escalation doesn’t give the body enough time to adjust, often leading to more intense GI symptoms. Most side effects peak during the first 90 days of treatment and then improve once the patient is on a stable, maintenance dose. Following a "low and slow" approach – starting with a small dose and gradually increasing it – allows the digestive system to adapt and significantly reduces discomfort.
How GLP-1 Medications Affect Digestion
Delayed Stomach Emptying and Nausea
GLP-1 medications play a key role in digestion by acting as an enterogastrone, triggering what’s known as the "ileal brake" mechanism. This process slows the movement of food from the stomach to the intestines, helping to prevent the lower digestive tract from becoming overwhelmed by too many calories at once. They achieve this by stimulating the pyloric sphincter and reducing peristalsis, which extends the time food remains in the stomach.
This effect is largely mediated through the vagal nerve, the critical connection between the brain and digestive system. Research has shown that blocking this nerve eliminates the stomach-slowing effect entirely. For example, studies on liraglutide revealed that 57% of patients experienced delayed gastric emptying, though nearly half saw this normalize after 16 weeks of use. GLP-1 medications can even double the time it takes for the stomach to empty half of its contents.
"Although slowed gastric emptying is integral to reducing post-prandial blood glucose responses… marked slowing… might also increase the propensity for longer intragastric retention of food." – PubMed Abstract
Nausea is another common side effect, stemming from prolonged food retention in the stomach and the medication’s impact on the brain. GLP-1 drugs target the Area Postrema and dorsal vagal complex, brain regions that control vomiting and food aversion. Interestingly, the nausea they cause isn’t necessary for weight loss, as these effects are managed by brain cells separate from those regulating feelings of fullness. One difference worth noting: short-acting drugs like exenatide maintain their stomach-slowing effects over time, while long-acting drugs like semaglutide tend to show reduced effects after about two weeks, as the body adapts to continuous receptor stimulation.
Beyond the stomach, these medications also influence intestinal activity, contributing to a range of symptoms.
Changes in Intestinal Movement
In the small intestine, GLP-1 medications reduce both migratory motor complexes and post-meal contractions. In the colon, they inhibit circular muscle contractions, slowing the passage of food. These changes explain the range of gastrointestinal symptoms patients experience, from diarrhea to constipation.
Diarrhea often occurs due to reduced nutrient absorption, particularly fats, which creates an osmotic effect that draws water into the intestines. GLP-1 medications also decrease pancreatic enzyme secretion – reducing enzymes like trypsin and lipase by over 40% – further impairing fat digestion. In the SURPASS clinical trials, 12% to 22% of participants on tirzepatide reported diarrhea.
On the flip side, constipation results from reduced colonic contractions, which slow transit time excessively. For instance, semaglutide users face a relative risk of 2.10 for constipation compared to placebo, while tirzepatide users have an even higher relative risk of 3.36. These intestinal side effects are typically most pronounced during dose escalation and tend to improve as the body adjusts.
Effects on the Gallbladder
GLP-1 medications also impact the gallbladder by reducing CCK-induced contractions, which are necessary for proper bile emptying. Studies with exenatide demonstrated that even a single dose could significantly reduce gallbladder contractions in healthy individuals. This slowed emptying, combined with changes in bile metabolism – such as lower bile acid production and increased excretion – creates conditions that make gallstone formation more likely.
The risk of gallstones becomes especially concerning during periods of rapid weight loss, a primary goal of GLP-1 therapy. Rapid weight loss prompts the liver to release more cholesterol into bile while the gallbladder empties less frequently, creating the perfect environment for stones to form. A 2025 meta-analysis found that semaglutide increased the relative risk of cholelithiasis (gallstones) by 1.92, liraglutide by 1.75, and tirzepatide by 1.36. Additionally, liraglutide was linked to a relative risk of 12.52 for acute cholecystitis, though this wasn’t statistically significant across all patient groups.
While gallbladder-related issues are less common compared to other gastrointestinal side effects, they can cause significant discomfort for some patients, particularly during the dose-escalation phase and periods of rapid weight loss.
sbb-itb-e2779c3
Research on Specific GI Symptoms
Recent research sheds light on how GLP-1 receptor activation triggers distinct gastrointestinal symptoms.
Nausea and Vomiting
Nausea and vomiting are the most commonly reported side effects of GLP-1 medications. A meta-analysis of 48 trials involving 27,729 participants found that 21.49% experienced nausea, while 9.10% reported vomiting.
These symptoms tend to follow a predictable pattern. For instance, in the STEP 2 trial, nausea from semaglutide rose from 5% at week 1 to 15% by week 13, then decreased to 8% by week 68. Real-world data from the FDA Adverse Event Reporting System shows that 77.44% of gastrointestinal side effects occur within the first 30 days, with a median onset time of just 1 day.
The risk of nausea and vomiting varies across medications. A 2025 network meta-analysis ranked nausea risk as follows: orforglipron (highest, relative risk 4.77), liraglutide (3.09), semaglutide (2.94), tirzepatide (2.89), exenatide (2.66), and cagrilintide (2.29). For vomiting, tirzepatide posed the highest risk (relative risk 13.22), followed by semaglutide (4.21) and liraglutide (3.87). Interestingly, the SURPASS-2 trial found that patients on tirzepatide 5 mg experienced less nausea (17.4%) and vomiting (5.7%) compared to those on semaglutide 1 mg, who reported 19.2% nausea and 8.1% vomiting, despite tirzepatide leading to greater weight loss.
"Nausea/vomiting by week 12 (end of dose escalation) or throughout treatment contributed minimally (<0.1 kg) to the superior weight loss with semaglutide versus GLP-1RA comparators." – Diabetes Therapy
While these symptoms can be unpleasant, they generally subside as the body adjusts to treatment and have minimal impact on overall weight loss. Next, we’ll look at how delayed gastric emptying contributes to bloating and abdominal discomfort.
Bloating and Abdominal Discomfort
Bloating and abdominal discomfort often stem from delayed gastric emptying, which keeps food in the stomach longer than usual. This delay increases abdominal pressure and distention. In some cases, slowed intestinal motility may lead to small intestinal bacterial overgrowth (SIBO), further contributing to bloating and gas.
Certain medications carry a higher risk of abdominal symptoms. Tirzepatide, semaglutide, and liraglutide are linked to increased rates of abdominal pain and distention. Notably, real-world data associate liraglutide with a strong likelihood of upper abdominal pain, showing a reporting odds ratio of 4.63.
These symptoms are most noticeable during the first 12 weeks of treatment, often referred to as the dose-escalation phase. Around 6% to 10% of patients stop treatment due to gastrointestinal side effects, and about 15% require dose adjustments.
Delayed gastric emptying also influences other symptoms, such as diarrhea and constipation, which we’ll discuss next.
Diarrhea and Constipation
Both diarrhea and constipation are frequent side effects of GLP-1 medications. Among patients with type 2 diabetes, diarrhea occurs in about 10.62% of cases, while constipation affects 7.92%. These symptoms typically appear early in treatment, with over 77% reported within the first month.
The timing of symptom onset varies by medication. Semaglutide has a median onset of 4 days, liraglutide 3 days, and dulaglutide and exenatide around 1 day. Tirzepatide carries the highest risk of diarrhea in type 2 diabetes patients, while semaglutide has the highest risk for constipation. Additionally, liraglutide is linked to the highest rate of severe gastrointestinal side effects (23.31%), while dulaglutide has the lowest (12.29%).
| Medication | Diarrhea Risk | Constipation Risk | Median Onset |
|---|---|---|---|
| Tirzepatide | Highest (~15%) | Very Low (0.14%) | N/A |
| Semaglutide | High (10.6%) | Highest (8%) | 4 days |
| Liraglutide | Moderate (6.5%) | Moderate (7%) | 3 days |
| Dulaglutide | Moderate (8%) | Moderate (6%) | 1 day |
| Exenatide | Low (7%) | Lowest (6%) | 1 day |
"Gastrointestinal toxicities tended to occur early after treatment initiation with fluctuation over time, both in a type 2 diabetic population and a more general population." – Lulu Liu, Researcher, West China Second University Hospital
There’s a noticeable difference between short-acting and long-acting formulations. Long-acting medications like semaglutide and tirzepatide tend to report higher rates of both diarrhea and constipation compared to short-acting options like exenatide. Semaglutide’s longer half-life – about 168 hours compared to liraglutide’s 13 hours – may contribute to the extended duration and prevalence of these side effects.
What Patients Need to Know
Navigating side effects and knowing when to seek help can greatly improve your experience with GLP-1 medications.
Managing Mild Side Effects
To ease gastrointestinal discomfort, start with gradual dose increases. Adjusting your diet can also help manage symptoms. Stick to small, low-fat meals like toast, crackers, rice, or oatmeal, and steer clear of greasy or sugary foods. Dr. Jaime Almandoz, a Weight Management Specialist at UT Southwestern Medical Center, advises:
"If you feel nauseous right now, ‘don’t feed the nausea.’ Adding more food may make your stomach feel like a rock."
Cold foods, such as fruit plates or chicken salad, tend to have milder odors compared to hot meals, which can be easier to tolerate.
Staying hydrated is key, especially if you’re dealing with vomiting or diarrhea. Aim for at least 64 ounces of fluids daily. Options like ice-cold drinks or warm ginger and lemon teas can soothe your stomach. For constipation, increase your fiber intake to 25–38 grams per day, paired with plenty of water. If diarrhea is an issue, avoid dairy, coffee, and chocolate. Over-the-counter aids, such as stool softeners or anti-nausea medications, might help, but check with your healthcare provider before using them.
Simple lifestyle changes can also make a difference. Avoid lying down immediately after eating and take a short walk instead to aid digestion. Clinical trials show that nausea typically lasts about 8 days, while vomiting subsides within 2 days, so these symptoms often improve as your body adjusts.
If these steps don’t provide relief, it’s important to know when to take further action.
When to Seek Medical Help
While most side effects are manageable, some symptoms demand immediate medical attention. Contact a healthcare provider if you experience persistent vomiting or diarrhea, severe abdominal pain, jaundice, or if you’re unable to pass gas or have a bowel movement. These symptoms could indicate serious conditions like pancreatitis, bowel obstruction, or gallbladder disease.
The FDA has reported 90 cases of ileus (bowel obstruction) linked to GLP-1 medications, leading to updated warnings on medication labels. Severe dehydration from vomiting and diarrhea can also result in acute kidney injury for some patients. If symptoms occur during a dose increase, consult your doctor about staying on your current dose longer before escalating.
The Importance of Personalized Care
Self-care is important, but personalized medical guidance is essential for balancing the benefits of weight loss with manageable side effects. Adjusting doses and monitoring symptoms should be tailored to each patient. Dr. Michael Camilleri, a Consultant in Gastroenterology and Hepatology at Mayo Clinic, emphasizes:
"If the patient is developing symptoms, we need to ask, ‘Do those symptoms reflect an impairment of the stomach or intestinal function?’ And if so, then manage accordingly."
Programs like TrimRX offer personalized support to help patients handle dose adjustments effectively. Through tailored consultations, custom dosing, and ongoing care, patients can fine-tune their treatment plans. Dr. Supriya Rao, a Board-certified Physician in Internal Medicine and Gastroenterology, explains:
"We want to find a right balance between weight loss and symptoms you can manage."
TrimRX provides a range of GLP-1 options, including injectable semaglutide starting at $199 per month and dual-action GLP-1 + GIP medications starting at $349 per month, with free delivery. This flexibility helps healthcare providers find the best medication and dose for your individual needs and goals.
Conclusion
GLP-1 medications work by slowing digestion and reducing appetite, but these mechanisms can lead to gastrointestinal (GI) side effects for as many as 40% of patients. The connection between delayed gastric emptying and altered intestinal movement highlights that these symptoms are not unexpected complications but rather a known part of how the therapy functions.
For most patients, GI issues tend to improve over time with proper adjustments. Since responses to treatment differ from person to person, personalized care is essential. It’s worth noting that over 10% of patients may pause or stop treatment due to side effects, emphasizing the need for tailored medical approaches.
"Management comes down to individualizing the experience of the patient." – Dr. Michael Camilleri, Mayo Clinic
Working closely with healthcare providers to adjust doses, address complications, and refine dietary plans can help patients stay on track with their treatment. Flexible titration schedules and ongoing support programs can make a big difference in managing side effects while achieving sustainable weight loss. The goal is to find a balance where the benefits of the medication outweigh the manageable side effects, allowing most patients to stay on therapy and experience its positive outcomes.
This underscores the importance of individualized treatment strategies to ensure both effectiveness and tolerability.
FAQs
How can I reduce nausea when starting GLP-1 medications?
Nausea is a frequent side effect when starting GLP-1 medications. These drugs slow down digestion and help you feel fuller, which can lead to some stomach discomfort. To help manage this, here are a few tips:
- Begin with a lower dose and gradually increase it as directed by your healthcare provider.
- Take the medication after eating a light snack to reduce its effect on your stomach.
- Opt for smaller, low-fat meals and steer clear of heavy or greasy foods, which can make nausea worse.
- Keep hydrated by sipping on water or clear fluids throughout the day.
If the nausea doesn’t improve, reach out to your healthcare provider. They might adjust your dosage, suggest anti-nausea medication, or offer other solutions to help you stay on track with your treatment while still reaping its benefits for weight loss and blood sugar management.
What should I do if I have severe gastrointestinal side effects from GLP-1 medications?
If you’re dealing with severe gastrointestinal issues such as ongoing nausea, vomiting, intense bloating, or diarrhea, it’s crucial to stop taking your medication and contact your healthcare provider right away. They might suggest pausing the treatment, adjusting your dosage, or revising your medication schedule.
In the meantime, focus on staying hydrated by sipping water or oral rehydration solutions. Stick to small, bland meals – think toast or crackers – and steer clear of fatty or spicy foods. For nausea, remedies like ginger might help, but only use them if your provider has given the green light.
If symptoms escalate to persistent vomiting, signs of dehydration (such as a dry mouth, dizziness, or reduced urine output), severe abdominal pain, or if you notice blood in your stool or vomit, seek immediate medical attention. For those enrolled in TrimRX’s program, their clinical support team is available for quick assistance and tailored advice.
Lastly, never restart or increase your medication dosage without explicit approval from your healthcare provider.
What dietary changes can help manage side effects from GLP-1 medications?
Yes, making small changes to your diet can go a long way in reducing common gastrointestinal (GI) side effects, like nausea and bloating, often linked to GLP-1 medications. Experts suggest eating smaller, more frequent meals and sticking to low-fat, mild, and easy-to-digest foods. Large meals should be avoided since these medications slow down stomach emptying, which can make discomfort worse.
A well-rounded diet featuring lean proteins (like chicken, fish, or tofu), non-starchy vegetables, fruits, and whole grains can help ease symptoms. Steering clear of greasy, fried, or heavily spiced foods, as well as carbonated drinks, can also reduce nausea and bloating. Simple habits like staying hydrated, sipping on ginger or peppermint tea, and sitting upright for about 30 minutes after meals can make a noticeable difference too.
For those seeking a more tailored solution, TrimRX provides personalized weight-loss programs that include meal planning tips to help manage side effects while supporting overall health goals.
Related Blog Posts

Transforming Lives, One Step at a Time
Keep reading
How to Adjust Weight Loss Goals on GLP-1 Medications
Adjust weight goals on GLP-1 meds by tracking body composition and labs, optimizing protein, activity, sleep, and working with your provider on dosing.
Falsified Mounjaro pens prompt urgent safety advisory
MHRA warns of counterfeit Mounjaro pens (batch D873576); stop use and check batch numbers for infection risk.
Novo Nordisk shares drop as Alzheimer’s hopes for weight-loss drug fade
Novo Nordisk’s semaglutide failed to slow Alzheimer’s in large trials, prompting shares to fall and expert reactions.



